Thomas Münzel MD, Omar Hahad PhD and Andreas Daiber PhD discuss the link between noise and cardiovascular disease, in this report about their research in the field
“One day man will have to fight the noise as fiercely as cholera and plague,” predicted Nobel prize winner Robert Koch in 1910. In fact, the spectrum of diseases has changed significantly in recent decades, so that currently non-communicable, often chronic, diseases such as cardiovascular diseases account for a significant proportion of the global burden.
There is annually a loss of more than one million healthy life years in Western Europe, measured on the basis of disability-adjusted life years, due to traffic noise-induced diseases (3). In recent years, noise research has made substantial progress, particularly with regard to relevant clinical studies as well as pathophysiological mechanisms that may play an important role in noise-induced cardiovascular effects, so that reviewing the current literature is essential.
Noise reaction model
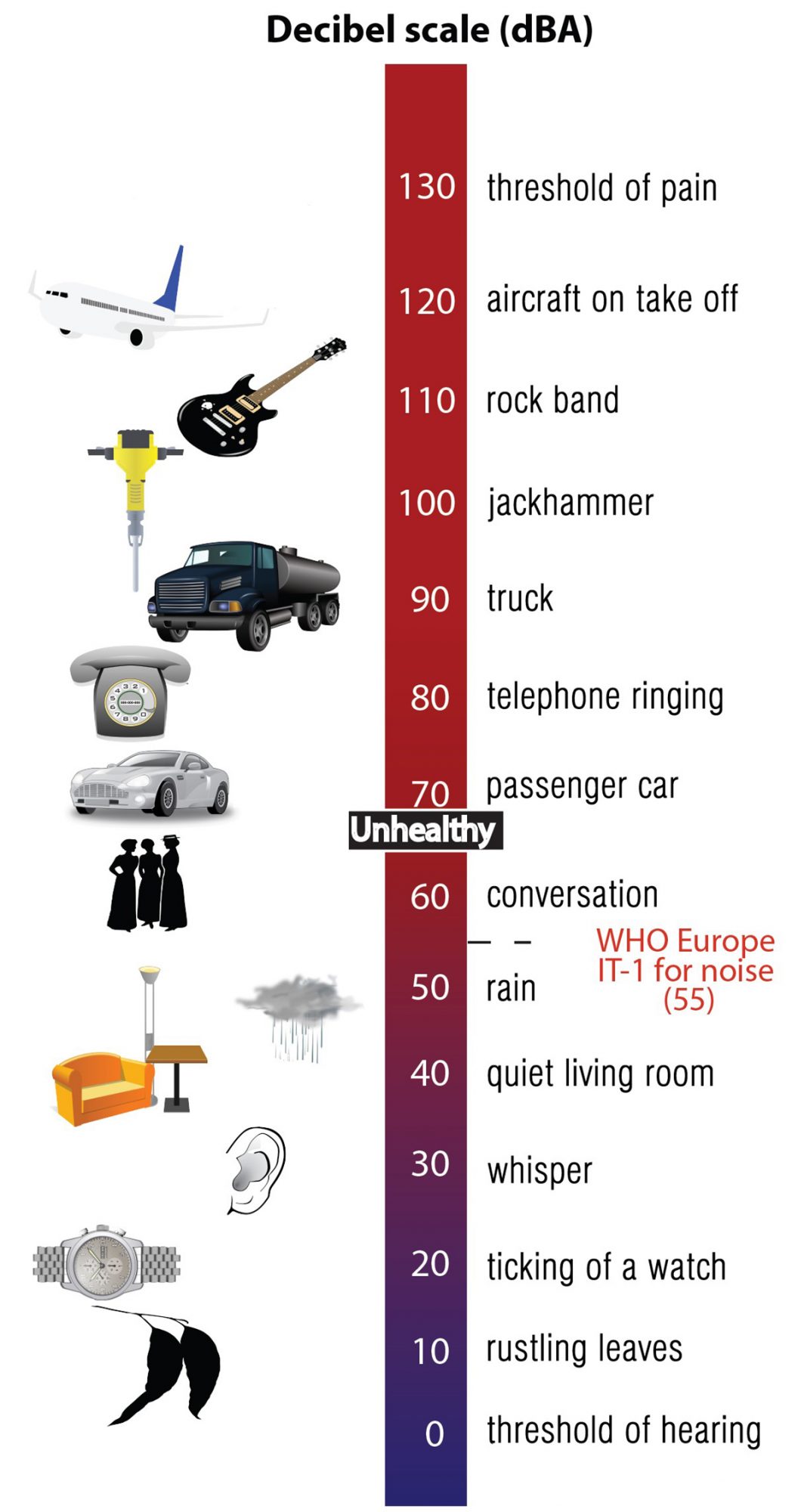
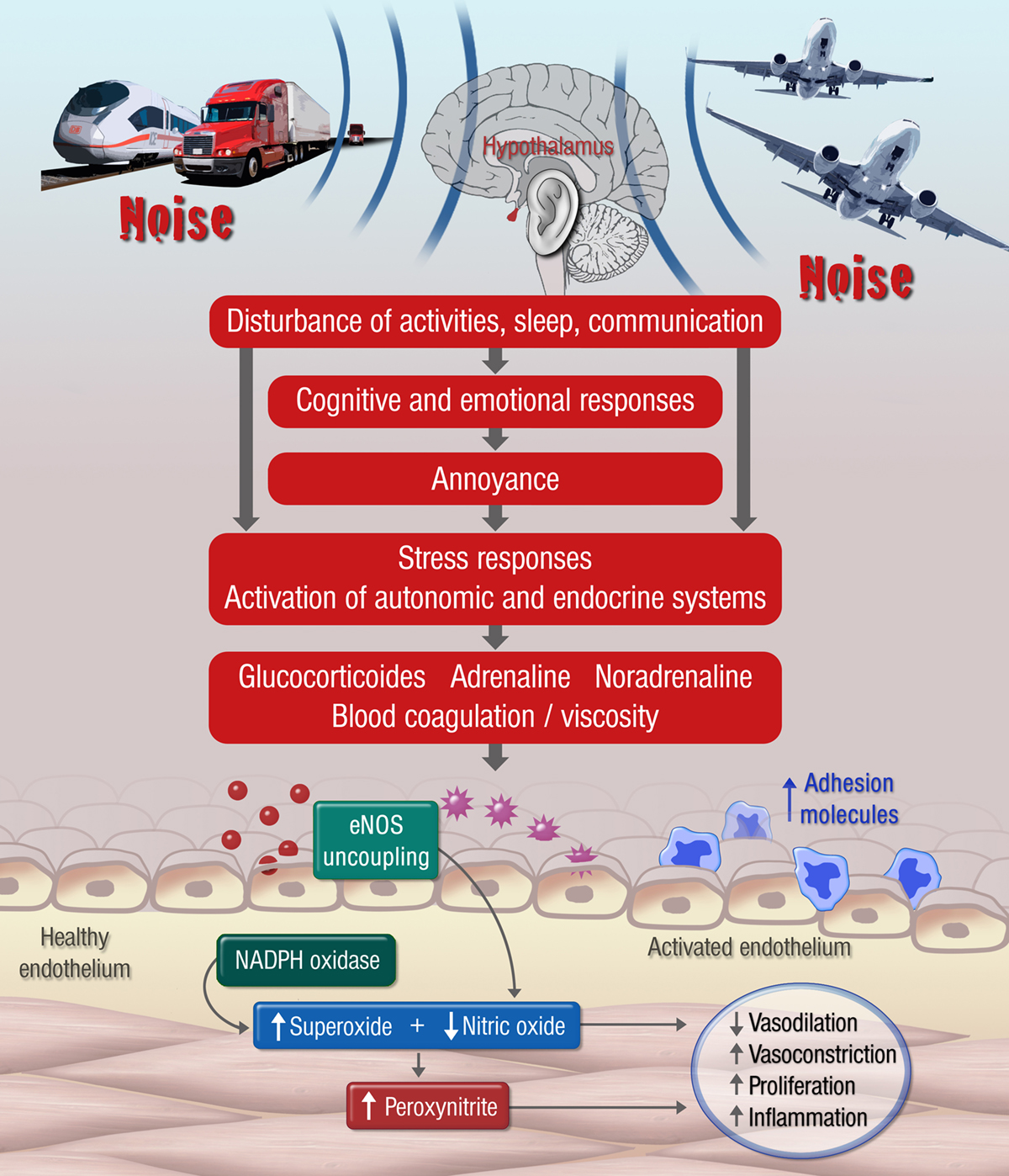
Noise is defined as disturbing sound with an objectively (physically) quantifiable dimension expressed as sound levels or decibel (dB (A)) and a subjective (psychological) dimension determined by the individual evaluation of the sound source by the listener (Figure 1). The so-called noise reaction model implicates that besides the direct auditory effects of noise on the organism (for example hearing damages caused by exposure to very high sound levels), the non-auditory noise effects are the main cause of a subsequent stress cascade (Figure 2).
In this sense, acute and chronic exposure to environmental noise may trigger stress and annoyance reactions, mediated through disturbances of sleep, communication and activities. These cognitive and emotional reactions lead to activation of the autonomic (sympathetic) and endocrine system (e.g., increased levels of catecholamines and cortisone) and, as a consequence, may contribute to an increased risk of developing cardiovascular disease via adverse changes in lipid and glucose metabolism and blood pressure regulation (Figure 2).
As mentioned before, noise is not only a physical stimulus expressed as sound levels but an individually experienced burden, which is accompanied by a variety of cognitive and emotional reaction patterns in case of inadequate coping. Noise-induced annoyance has been reported to play an important role in the development of noise-induced cardiovascular disease. Noise-induced adverse health effects primarily depend on the extent to which noise is perceived as disturbing (4, 5).
Data from a large prospective cohort study, the Gutenberg Health Study (N = 15,010, conducted at the University Medical Center Mainz) demonstrate that noise-induced annoyance caused by various sources during the day and at night, including aircraft, road traffic and railway noise, is dose-dependently associated with an increased risk of atrial fibrillation (6). Furthermore, in the Gutenberg Health Study it has been shown that the risk of depression and anxiety increases with increasing noise annoyance (6, 7), which in turn may negatively affect the cardiovascular system.
Epidemiological evidence on the relationship between noise and cardiovascular disease
Due to the increasing demand for mobility in recent years, the scientific assessment of noise-induced health effects in the population comes into focus. The quantity and quality of epidemiological research have improved substantially in recent years with regard to standardisation and estimation of noise exposure, consideration of larger study populations and improvement of adjustment for confounding variables. In addition, conditions such as habituation, sensitisation, conditioning and fatigue are adequately represented in the context of natural living conditions in epidemiological studies. The most important studies focus on coronary heart disease, myocardial infarction, stroke and arterial hypertension.
Stable coronary heart disease
Three meta-analyses showed that traffic noise leads to a significant increase in coronary heart disease (8-10). A meta-analysis from 2015 by Vienneau et al. included studies on the relationship between aircraft and road traffic noise and incident risk of coronary heart disease (8). A pooled relative risk (RR) of 1.06 was found starting at 50 dB (A) and per 10 dB (A) increase Lden (weighted day (7 a.m to 7 p.m), evening (7 p.m to 11 p.m), night (11 p.m to 7 a.m) level over a period of 24 hours, with a penalty of 5 dB (A) for the evening hours and 10 dB (A) for the night hours). This effect persisted after further adjustment for air pollution (mainly nitrogen oxide (NOX) or nitrogen dioxide (NO2) which were assessed in a subgroup of studies) and after exclusion of studies with no information on smoking status. A meta-analysis of Babisch reached a similar result (RR 1.08) starting at 52 dB (A) and per 10 dB (A) increase Lden (weighted day, night level over a period of 24 hours, with a penalty of 10 dB (A) for the night hours) road traffic noise (9).
In a recent meta-analysis from 2018 conducted by the WHO, the analysis of longitudinal studies showed that road traffic noise increased the risk of incident coronary heart disease by 8%, starting at 50 dB (A) and per 10 dB (A) increase Lden (10). Since increasing volumes of traffic is not only a concern in terms of noise exposure but also lead to an increased air pollution load, a differentiation of both variables is needed in order to distinguish between effects. Despite the high correlation of both variables, noise and air pollution are considered to have independent and adverse effects on the cardiovascular system (11).
Acute myocardial infarction
Further cohort studies with comprehensive adjustment for air pollution, socioeconomic status and lifestyle factors have found a significant relationship between road traffic noise and the incidence of myocardial infarction (12, 13). Data from a large Danish cohort (N = 50,744) showed that road traffic noise exposure (10-year average) was associated after adjustment for NO2 levels with increased risk of myocardial infarction with a hazard ratio (HR) of 1.12 per interquartile range Lden (12).
Similar results were found for a Swedish cohort (odds ratio 1.38) for road traffic noise (13). A nationwide Swiss cohort study (N = 4,415,206) investigated the impact of aircraft, road traffic and railway noise on cardiovascular mortality (14). The strongest relationships after adjustment for NO2 levels were found for mortality due to myocardial infarction with an HR of 1.038 for road traffic, 1.018 for railway and 1.026 for aircraft noise starting at 30 (rail and aircraft noise) or 35 dB (A) (road traffic noise) and per 10 dB (A) increase.
In a further analysis of a Danish cohort (N = 57,053), road traffic noise exposure increased the risk of incident myocardial infarction by 12% starting at 42 dB (A) and per 10 dB (A) increase Lden after adjustment for NOX levels, smoking status, education and diet (15).
Stroke
Based on a large-scale cohort study (N = 57,053), Sørensen et al. established that road traffic noise, independent of NOX levels, smoking status, diet and alcohol consumption, increased the risk of stroke by 14% starting at 55 dB (A) and per 10 dB (A) increase Lden (16). A further large-scale study including 3.6 million residents around London Heathrow Airport showed that aircraft noise during day (7 a.m to 11 p.m) as well as during night (11 p.m to 7 a.m) was dose-dependently associated with increased hospitalisation after stroke after control for age, sex and lifestyle factors with a higher hospitalisation risk for noise during day than night (17).
Similar results were found in the same study for mortality after stroke, even after adjustment for particulate matter exposure (PM10 – particles less than 10 micrometres in diameter). These results indicate that in particular night-time aircraft noise is associated with the adverse effects on the cardiovascular system. Another study that included 8.6 million residents of London found that road traffic noise was associated with an increased risk of stroke-related hospital admission (18).
In addition, the study could demonstrate that road traffic noise (>60 vs. <55 dB (A)) during the day was significantly associated with increased all-cause mortality in adults.
Arterial hypertension
A meta-analysis of 24 studies showed that road traffic noise is associated with an increased risk of hypertension starting at 45 dB (A) and per 5 dB (A) increase (19). However, since this analysis only included cross-sectional studies, the causal interpretation is limited. In further large-scale prospective studies, however, a relationship between aircraft and road traffic noise exposure and increased risk of hypertension could be demonstrated (20-22), with a higher impact for night-time aircraft than for road traffic noise (22).
Mechanistic insight from translational studies
There are only a few studies that provide mechanistic insight into the relationship between noise exposure and markers of cardiovascular risk. More recently, our group demonstrated that simulated night-time noise (30 and 60 flights/night, peak sound level of 60 dB (A), mean sound level of 43 and 46 dB (A), respectively) in healthy subjects and in patients with prevalent coronary heart disease is associated with worsening of vascular (endothelial) function (measured by flow-mediated dilation), increased stress hormone levels (epinephrine) and decreased sleep quality (23, 24).
Interestingly, the impairment of vascular function in healthy subjects was significantly improved by the single administration of vitamin C (2g, p.o. (23)). This suggests that increased oxidative stress was at least in part responsible for aircraft noise-induced impairment of endothelial function. Two recent animal studies could further reveal relevant molecular mechanisms by which noise induces vascular dysfunction (25, 26).
Hereby, Münzel et al. demonstrated that simulated aircraft noise exposure for four days led to a significant increase in stress hormone levels, increased blood pressure, changes in vascular wall gene expression and impaired vascular function, mainly due to an increased free radical formation and oxidative stress (25). With these studies, two important enzymes were identified being involved in the initiation of aircraft noise-induced vascular dysfunction: the nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase) and the nitric oxide synthase (NOS).
The noise-induced dysregulation of these enzymes enhanced the formation of reactive oxygen species, which directly led to decrease the vascular bioavailability of nitric oxide (NO), an important radical with powerful vasodilator and antiatherosclerotic properties and thus resulted in the impairment of endothelial function (Figure 2). Our group also demonstrated that in addition to vascular dysfunction, cerebral damage was notified when aircraft noise was applied during the sleep but not during the waking phase (26).
Thus, these findings confirm results from sleep research which demonstrated that short and fragmented sleep is associated with increased risk of cardiovascular disease (27). A recent WHO meta-analysis showed that traffic noise significantly increases the risk of sleep disorders, which may be a relevant factor in the development of cardiovascular disease (28). Results of the SAPALDIA study (Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults) also showed that the amount of traffic noise events, especially at night, is associated with increased arterial stiffness, an important marker of vascular dysfunction (29).
Summary and conclusions
Epidemiological studies could clearly demonstrate that traffic noise exposure is a significant risk factor for the development of cardiovascular disease. Current experimental studies emphasise that (in particular night-time) noise may induce vascular dysfunction triggered by the increased formation of free radicals, inflammatory processes and oxidative stress at the vascular and cerebral level, which in turn promote increased blood pressure and atherosclerosis.
These studies could identify crucial pathophysiological markers that may further allow the development of drug strategies in order to minimise the adverse effects of noise on the organism. The present results also show that traffic noise is a novel cardiovascular risk factor.
Considering the new WHO noise guidelines with recommendations for significantly lower noise levels during the day- and night-time (30), actions are needed that allow adequate protection against the adverse health effects of traffic noise and, in particular, noise during night-time.
Key messages
• Epidemiological studies show that traffic noise increases the risk of cardiovascular diseases such as arterial hypertension, coronary heart disease, myocardial infarction and stroke.
• Acute and chronic noise exposure trigger stress responses that lead to activation of the autonomic and endocrine system, initiating development of cardiovascular risk factors.
• Pathophysiologically, night-time traffic noise, in particular, induces oxidative stress and inflammatory processes at the cerebral level, which negatively affects the vascular system and lead to endothelial dysfunction and an increase in blood pressure.
• Traffic noise has to be acknowledged as an important risk factor for cardiovascular disease, a risk factor that cannot be modified by patients or doctors but rather by politicians introducing noise limits that protect the people from adverse cardiovascular effects by noise.
• Accordingly, more emphasis has to be put on the implementation of noise mitigation strategies.
Selected References:
1 Munzel T, Schmidt FP, Steven S, Herzog J, Daiber A, Sorensen M. Environmental Noise and the Cardiovascular System. J Am Coll Cardiol. 2018;71(6):688-97.
2 Munzel T, Sorensen M, Schmidt F, Schmidt E, Steven S, Kroller-Schon S, et al. The Adverse Effects of Environmental Noise Exposure on Oxidative Stress and Cardiovascular Risk. Antioxid Redox Signal. 2018;28(9):873-908.
3 Burden of disease from environmental noise – Quantification of healthy life years lost in Europe Copenhagen: World Health Organization. Regional office for Europe; 2011.
23 Schmidt FP, Basner M, Kroger G, Weck S, Schnorbus B, Muttray A, et al. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J. 2013;34(45):3508-14a.
24 Schmidt F, Kolle K, Kreuder K, Schnorbus B, Wild P, Hechtner M, et al. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol. 2015;104(1):23-30.
25 Munzel T, Daiber A, Steven S, Tran LP, Ullmann E, Kossmann S, et al. Effects of noise on vascular function, oxidative stress, and inflammation: mechanistic insight from studies in mice. Eur Heart J. 2017;38(37):2838-49.
26 Kroller-Schon S, Daiber A, Steven S, Oelze M, Frenis K, Kalinovic S, et al. Crucial role for Nox2 and sleep deprivation in aircraft noise-induced vascular and cerebral oxidative stress, inflammation, and gene regulation. Eur Heart J. 2018;39(38):3528-39.
30 WHO report: ENVIRONMENTAL NOISE GUIDELINES for the European Region. http://www.euro.who.int/__data/assets/pdf_file/0008/383921/noise-guidelines-eng.pdf?ua=1
A complete reference list can be requested from the corresponding author.
Abbreviations:
Lden: Day-evening-night level. It is a descriptor of noise level based on energy equivalent noise level (Leq) over a whole day with a penalty of 10 dB(A) for night time noise (22.00-7.00) and an additional penalty of 5 dB(A) for evening noise (i.e. 19.00-23.00).
Professor Thomas Münzel
University Medical Center of the Johannes Gutenberg-University Mainz
Center for Cardiology
Tel: +49 613 117 5991
tmuenzel@uni-mainz.de
*Please note: This is a commercial profile
Editor's Recommended Articles
-
Must Read >> Cardiovascular disease: How to stop a killer
-
Must Read >> Theories underpinning psychological practice ‘wrong’