Leo Braack, Malaria Consortium’s Senior Vector Control Specialist, recounts the ongoing battle against vector-borne diseases and shares why the need for new mosquito control tools has become critical
The tiny mosquito has had an outsize impact on humanity. Mosquitoes have caused the deaths of more people than were killed in all the wars ever fought. It also brought to a grinding halt the building of the Panama Canal. France, having won the contract to build the canal that would traverse Central America, started work in 1881, but by 1889 the project was brought to a standstill with more than 85% of workers killed or hospitalised by yellow fever and malaria. The project was abandoned for several years and when resumed by the United States, the discovery that Anopheles mosquitoes transmit malaria had been made and the role of Aedes mosquitoes in yellow fever was clarified. A major programme of mosquito control ensued, resulting in a dramatic reduction of disease and the canal was completed by 1914. Combatting mosquitoes focused on larval control, by way of draining ditches, marshes, Paris
Green larvicide and oil, spraying of pyrethrum, and screening of houses; these methods would remain the main manner of malaria and mosquito control for several decades, with large successes.
World War 2 brought with it major casualties due to malaria. But DDT – the first modern synthetic insecticide – had been developed during these years and its effectiveness was proven. The World Health Organization (WHO) launched the Global Malaria Eradication Program in 1955 and extraordinary efforts flooded much of the world with DDT, along with the hope of eradicating malaria once and for all. Large areas were cleared of malaria, but resistance developed within mosquitoes against DDT, which rapidly spread until it forced the WHO to abandon the ambitious eradication campaign in 1969. From then on, malaria ‘control’ would be the goal rather than eradication.
The tropical world battled on bravely while malaria surged back: India, for example, had reduced its malaria burden from over 75 million cases per annum in the 1940s to about 100,000 in the late 1960s, but could not fully stem re-bounding malaria. Thankfully, a new generation of insecticides emerged, and together with new applications reinvigorated hope. Synthetic pyrethroids, incorporated into bed nets as Long-Lasting Insecticidal Nets (LLINs) or sprayed onto the walls of domestic dwellings as Indoor Residual Spraying (IRS) suggested that, with greater funding and organisation, malaria could be beaten. The Roll-Back Malaria Alliance of partners was established in the late 1990s, to be joined a few years later by the Bill & Melinda Gates Foundation, and with the support of the WHO, once more they adopted the goal of global eradication. Well over a billion bed nets were distributed, and excellent successes were achieved in reducing the malaria burden over the period 2000 to 2015.
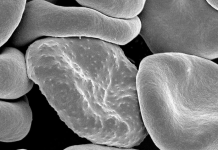
Inevitably, however, mosquito populations began developing genetic modifications that enabled them to avoid the toxic effects of the insecticides. Equally ominous, more and more mosquito populations adapted to bite outdoors and in the early hours of the night or morning, where the protective effects of bed nets or indoor spraying could not reach. And so, from about 2015, the downward trend of malaria case numbers flattened to a plateau, and in many places started to rise again.
An uphill battle towards elimination
So, we find ourselves in a hold situation, keeping the pressure on malaria, making slow gains and in a very few countries achieving elimination, but fighting an uphill battle. Much of the remaining malaria transmission across the globe is now outdoors and we do not have effective tools to confront these mosquitoes on their new battleground. We have to continue to protect people sleeping indoors, and those nets and treated walls do whittle away at the mosquitoes that periodically venture indoors. But for impoverished, rural people that cook, eat and socialise outdoors in the evenings or rise early for domestic chores, we are surprisingly ill-prepared to engage in a meaningful fight.
Repellents are the obvious answer, but for most rural poor regions, this is not sustainable. The WHO also does not endorse repellents because no one has proven that at the village scale it reduces malaria. Repellents may chase mosquitoes from one person, but they simply find another person to bite, and so the net effect is zero. Larviciding is supported by the WHO, to reduce populations of outdoor mosquitoes, but many of the vector mosquitoes breed in streams and extensive bodies of water difficult to treat, or in small pools hidden away by vegetation or nearby forest.
There are, however, several new tools under investigation that may help. Attractive toxic sugar baits: bait stations where mosquitoes can feed on sugary substances laced with toxic chemicals but covered with a protective layer so that honeybees and other ‘good’ insects will not be killed. There is also Ivermectin, which will kill mosquitoes that feed on blood from humans or cattle treated with the drug, for weeks after a single dose. Cattle are routinely treated with Ivermectin as a remedy against intestinal worms and with cattle a very common feature in malaria-endemic landscapes across the world, this is an exciting new approach, especially in contexts of residual malaria, where malaria ticks over at low incidence and is difficult to eliminate.
There are more technologically advanced methods available, some well-proven such as the release of millions of irradiated sterile male mosquitoes to flood the environment with laboratory-reared males that mate with wild females and result in sterile eggs. There is also the concept of ‘gene drive’, where genetically modified mosquitoes force a particular gene into the wild population and result in disease reduction. For Aedes mosquitoes that transmit viral diseases such as Dengue, Chikungunya and Zika, excellent results have been achieved in recent years through the release of laboratory-reared males implanted with the Wolbachia bacterium, a naturally-occurring intracellular organism that lives harmlessly in conjunction with their hosts. The males ‘donate’ the Wolbachia bacterium to females during mating and the bacterium becomes self-perpetuating. In Aedes, this method results in either reduced ability of the offspring to transmit virus or sterile eggs, depending on how the method is applied. But these techniques tend to be expensive and require special equipment, posing challenges for scaling up over large areas.
Closing thoughts on malaria
Globally, we are making slow headway in the fight against malaria, but there has been progress, nonetheless. Since 2000, 39 countries and territories have managed to rid themselves of malaria; the most recent is China. Existing tools can achieve local elimination, but the battle is becoming harder and mosquitoes and parasites are able to change their defences, which is why we too have to constantly adapt and respond with better tools and strategies.
We should also be on high alert; malaria has been distracting our attention from what will be our next global public health threat: mosquito-borne arboviruses such as Dengue, Chikungunya, Zika, Yellow Fever, West Nile Virus, Usutu, and a host of others few people have heard of. These arboviruses are spreading across the globe, each year more abundant. The mosquitoes that transmit them pose a different set of challenges, as most of them bite by day, with very different breeding habits. We must increase public awareness of the rising threat and invest much greater research effort to find ways to combat these viruses and mosquitoes.
Contributor Profile
Editor's Recommended Articles
-
Must Read >> Essential malaria parasite genes revealed