Researchers have identified circulating microparticle proteins with the ability to predict placenta accrete spectrum cases before their delivery, allowing improved mortality and morbidity for mothers
Roughly 50,000 out of 4 million births each year in the United States are shadowed by life-threatening conditions. According to Brigham and Women’s hospital, up to 900 of these result in maternal death during delivery.
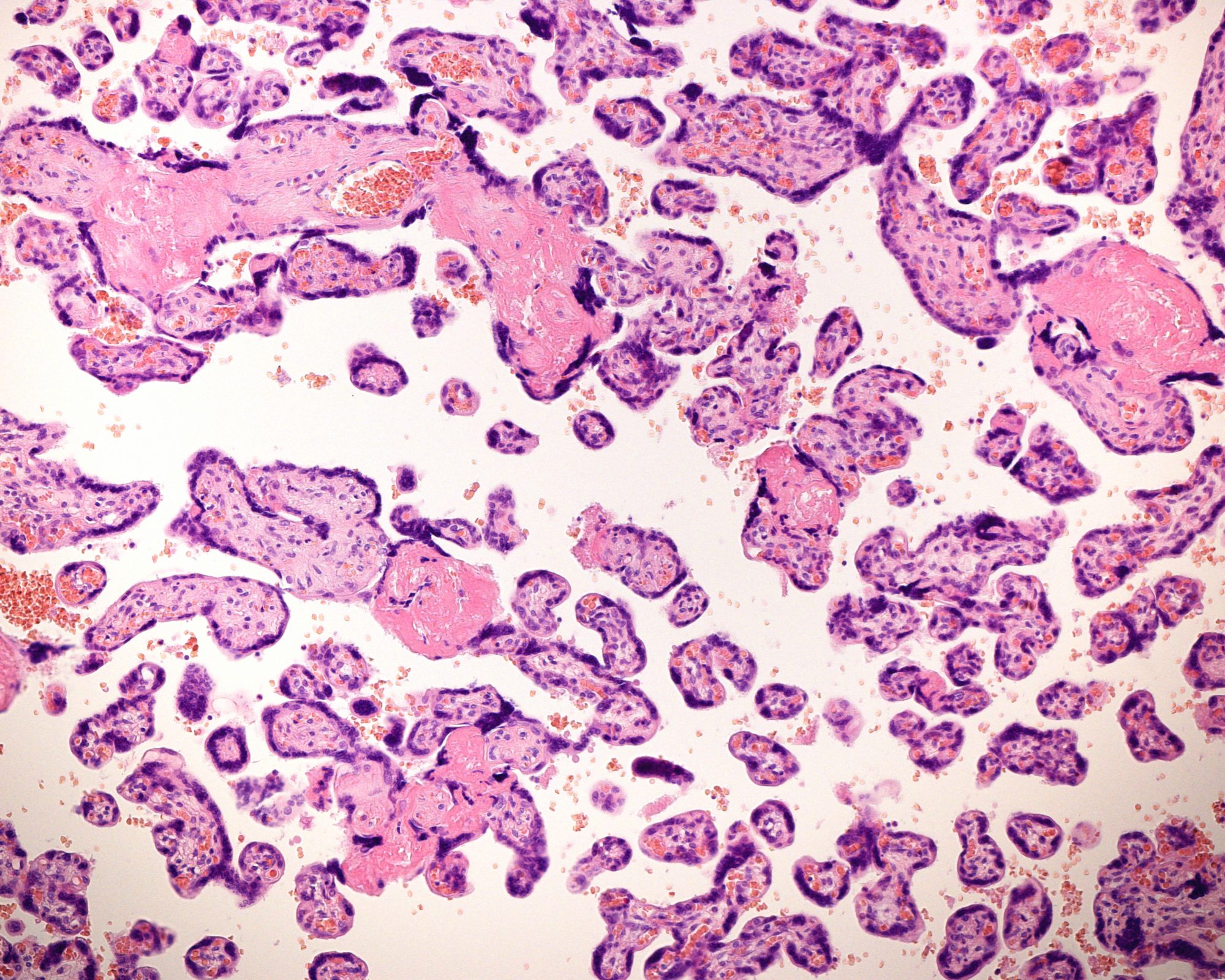
A major ongoing complication for those giving birth is placenta accreta spectrum (PAS). PAS are currently identified through ultrasounds, MRI and predictive confounding conditions, and although posing a threat to mother and child, these methods still leave between 33-50% of PAS cases undetected.
between 33-50% of PAS cases go undetected
Targeted test for predicting PAS
According to a new study by investigators from Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, there may be hope for a targeted test for predicting PAS during pregnancy. By finding more accurate predictions before labour occurs, healthcare professionals will be able to protect the lives of both parents and children on a wider scale.
By studying circulating microparticle (CMP) protein panels in pregnant women, the team identified five unique CMP proteins that can predict PAS as early as the second trimester of pregnancy.
Publishing their results in Scientific Reports, author Hope Yu, MD, a Maternal-Fetal Medicine physician, stated, “PAS is a significant contributor to maternal morbidity and mortality worldwide,” and that before the study “up to half of these cases weren’t able to be detected before delivery. [the] study aims to improve that detection rate using a blood test and to eventually improve health outcomes worldwide.”

Spectrum designation
Placenta accreta, a condition where the placenta attaches excessively into the uterine wall, gets its “spectrum” designation because of the varying degrees of placental penetration into the body that can occur. In some cases, the placenta attaches to the uterine muscle; in more severe cases, the placenta attaches through the uterine wall and to other organs, like the bladder. There are two major complications for PAS patients: abnormal placenta delivery after birth and heavy bleeding. Identification of PAS cases prior to delivery can help reduce and prepare for such complications.
There are two major complications for PAS patients: abnormal placenta delivery after birth and heavy bleeding
To identify PAS early, the team from Brigham looked to proteins associated with CMPs that are tiny, extracellular vesicles that cells use to communicate with one another and have been studied extensively in other disciplines since they provide a glimpse into cell crosstalk. The team set out to study CMPs at the maternal-fetal interface, with the goals of pinpointing a clinically useful PAS biomarker and investigating CMP mechanisms of PAS pathogenesis. The team’s primary goal was to construct a blood panel to identify PAS pregnancies.
The team conducted a nested case-control study with 35 PAS patients and 70 control patients, who were all retroactively diagnosed after delivery. CMP proteins were isolated and identified from patient plasma sampled during the second and third trimesters of pregnancy. In samples collected from patients who were 26 weeks pregnant, five CMP proteins distinguished PAS patients from control patients; at 35 weeks pregnant, four CMP proteins distinguished PAS patients from control patients. Additionally, in the second-trimester iron homeostasis and erythropoietin signalling were overrepresented — a trend that, in the third trimester, revealed abnormal immune function.
Successes in predicting placenta accrete
The study successfully identified five second-trimester CMP protein PAS indicators and four third-trimester CMP protein PAS indicators, enabling safe prediction of PAS well before delivery. The authors note that more research and clinical trials will be needed to further test the applicability of the protein panel. The next steps include widening the patient sample size and creating a standardized commercial test.
“It is so important to identify these cases prior to delivery,” said Yu. “If we can identify a PAS case during pregnancy, the patient can then make a potentially life-saving choice to deliver in a tertiary delivery centre with specialized providers. Having an experienced, multidisciplinary team by your side during a PAS birth can make an enormous difference when it comes to mortality and morbidity outcomes.”
Editor's Recommended Articles
-
Must Read >> Microplastics found in placenta and newborns
-
Must Read >> Maternal health: Vitamin D in pre-eclampsia