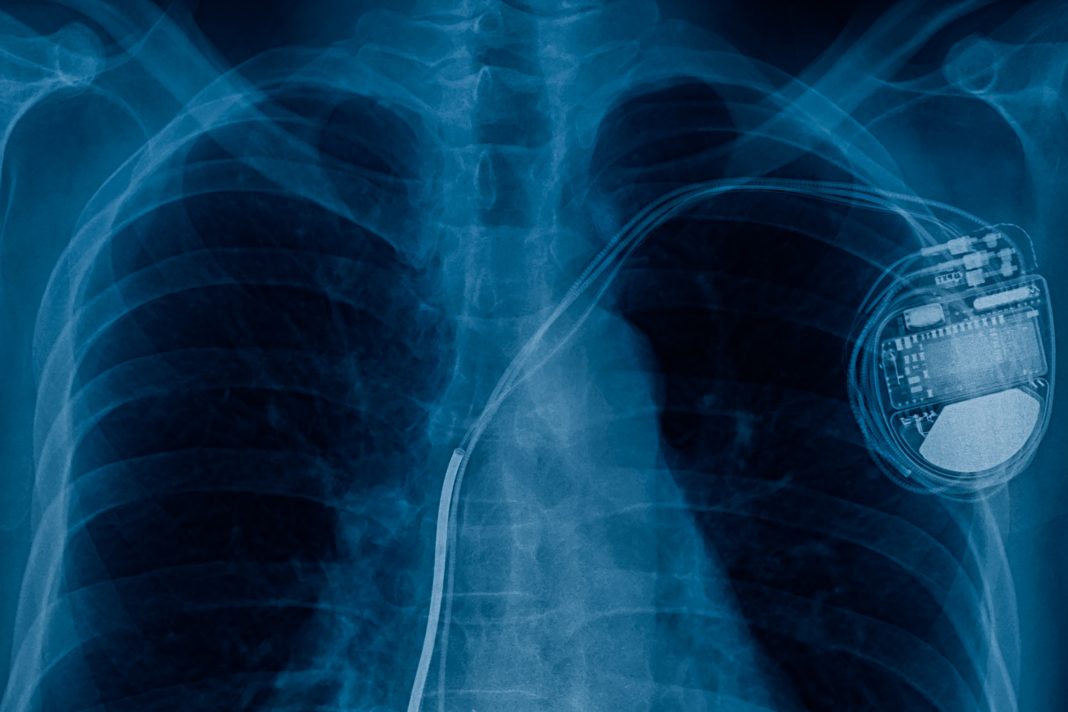
As the population ages, concerns about infections related to cardiac implantable electronic devices (CIEDs) are increasing. This article explores the risk factors and proposes potential solutions to improve the safety of cardiac devices
As the world’s population increases, the number of individuals aged 65 and over is expected to increase disproportionately, (1) which will likely lead to higher rates of pacemaker implantations (Cardiac Implantable Electronic Devices, or CIEDs). (2-4)
One of the complications associated with pacemaker implants is infection. In the first six months after the procedure, the infection rate is approximately 1% for pacemakers and 1.7% for defibrillators. Over two years, the infection rate rises to 9.5% for cardiac resynchronization devices. (5,6)
Reducing infections related to CIEDs is crucial, as in-hospital mortality rates for these infections range from 5% to 15%. (5,6)
While pacemakers effectively lower mortality and morbidity associated with cardiac arrhythmias, there are inherent risks associated with the procedures. (7)
These include early and late pocket infections, as well as an ongoing risk of pacemaker lead endocarditis within the right heart. In specialized centers, the rate of early device infections can decrease to less than 1% for CIED implants. (5,6) However, these infections carry a 5-15% risk of death, prolonged hospitalization, and significant financial costs. (5,6)
Factors increasing risk
Factors increasing risk are the complexity of the device and leads (e.g. cardiac resynchronisation pacemaker (CRTP) or defibrillator (CRTD) versus standard pacemaker), previous CIED procedures, previous CIED infections, atrial fibrillation, chronic kidney disease, chronic obstructive pulmonary disease, diabetes mellitus (particularly if poorly controlled), increased length of procedure, inexperienced implanter, insertion of a temporary pacemaker before implant of CIED, development of haematoma, and cardiomyopathy. (8-10)
Factors reducing risk
Factors reducing risk include prophylactic intravenous broad-spectrum antibiotics, shorter procedure time, experienced implanters, leadless pacemakers, antibiotic impregnated pouch (WRAP IT study), (11) procedures done in operating theatres rather than catheter laboratories, skin preparation with chlorhexidine rather than povidone iodine, hair shaving with electric clippers, laminar flow in the operating theatre. (8-10)
Leadless pacemakers
Leadless pacemakers have a much lower risk as the device is not physically touched before being implanted (12,13) however there are limitations to increased use of such devices, including limitation of applicable pacing sites, increased device cost compared to standard pacemaker, decreased battery longevity (but improved in such devices in 2025), inability to perform conduction system pacing or cardiac resynchronization pacing.
The increased competition from pacemaker manufacturers and the extended longevity of the new generation of leadless pacemakers are likely to reduce the implant cost and net yearly cost of leadless pacemakers. This needs to be balanced against the health and economic benefits of reduced morbidity and mortality from infections compared to pacemakers with leads.
Care must be taken to only implant CIEDs when clinically indicated. (14, 15) In my own practice, I have come across occasional patients with inappropriate pacemaker implants, some of whom have had life-threatening pacemaker-related infections.
Extravascular systems
Extravascular systems eliminate the risk of pacemaker lead endocarditis (e.g. subcutaneous rather than transvenous defibrillator system), but do not eliminate the risk of pacemaker pocket infections. (16)
Novel techniques
Novel techniques such as the WISE system (the WISE CRT system uses a leadless LV endocardial pacing electrode stimulated with ultrasound energy from a subcutaneous transmitter and battery; this requires existing conventional pacemaker leads in the heart). (17)
Further research into leadless pacemaker systems needs to be encouraged. Options include pacing nodules implanted within the myocardium, the implantation of stem cells trained to function as pacemaker cells, and in vivo genetic modification of cells within the myocardium to act as pacemaker cells. (18)
References
- Hannah Richie, Lucas Rodes-Guirao, Edoaurd Mathieu, et al. Population Growth: Our World in Data
- Mond HG, Proclemer A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009–a World Society of Arrhythmia’s project. Pacing Clin Electrophysiol. 2011 Aug;34(8):1013-27. doi: 10.1111/j.1540-8159.2011.03150.x. Epub 2011 Jun 27. PMID: 21707667.
- L.M deVries, W A Dijk, CA M Hooijschuur, MJG Leening, et al. Utilisation of cardiac pacemaker over a 20 -year period: Results from a nationwide pacemaker registry. Netherlands Heart Journal. 2017; 25: 47-55.
- Pamela Bradshaw, Paul Stobie, Matthew W Knulman, et al. Trends in the incidence and prevalence of cardiac pacemaker insertion in an ageing population. Open Heart 2014 Dec 10; 1(1):e000177. doi: 10.1136/ openhrt-2014-000177
- Michael Doring, Sergio Richter, Gerhard Hindricks. The Diagnosis and Treatment of Pacemaker Associated Infection. Dtsch Arzte int: 2018 Jun29; 115(26):445- 452. doi:10.3238/artzebl.2018.0445
- Han HC, Hawkins JM, Pearman CM, et al. Epidemiology of cardiac implantable electronic device infections: incidence and risk factors. Europace 2021; 23 (Suppl4): iv3-iv10.
- Ganesan AN, Moore K, Horton D, et al. Complications of cardiac implantable electronic device placement in public and private hospitals. Intern Med J 2020; 50: 1207-1216.
- Blomstrom-Lundquist C, Traykov V, Erba PA et al. European Heart Rhythm Association (EHRA) international consensus document on how to prevent, diagnose, and treat cardiac implantable electronic device infections – endorsed by the Heart Rhythm Society (DRS), the Asia Pacific Heart Rhythm Society (APHRS), the International Society for Cardiovascular Infectious Diseases (ISCVID), and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 202; 41: 2012-2032
- Klug D, Balde M, Pavin D, et al. PEOPLE Study Group. Risk factors related to infections of implanted pacemakers and cardioverter-defibrillators. Circulation 2007; 116: 1349-1355.
- Shawon MSR, Sotade OT, li L, et al. Factors associated with cardiac implantable electronic device-related infections., New South Wales. 1016-2021. A retrospective cohort study. Med J Aust 2024: 220:510-516.
- Wilkoff BL, Boriani G, Mittal S et al; WARP-IT Investigators. Impact of cardiac implantable electronic device infection: a clinical and economic analysis of the WRAP-IT trial. Circ. Arrhythm Electrophysio. 2020; 113: e008280.
- Toshimasa Okabe, Muhammad R Afzal, Mahmoud Houmse, et al. Tine-Based Leadless Pacemaker. JACC: Clinical Electrophysiology. 202:6: 1318-1331.
- Apostolos Ilias Vouliotis, Paul P Robers, Polychronis Dilaveris, et al. Leadless Pacemakers: Current Achievements and Future Perspectives. Eur Cardiol. 2023 Aug 18;18:e49. doi: 10.15420/ecr 2022.32
- William F Heddle: Averting infections when implanting cardiac pacemakers and defibrillators. Medical Journal of Australia 220; issue 10; 507-508. doi.org/10.5694/mja2.52305
- Glickson M, Nielsen JC, Kronborg MB, et al; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J 2021; 42: 3427-3520J
- Knops RE, Olde Norkamp, P-P. H M Delnoy, et al. Subcutaneous or Transvenous Defibrillator Therapy. N Engl J Med 202; 383: 526-536.
- Jagneet P Singh, Christopher A Rinaldo, Prashanthan Sanders, et al. Leadless Ultrasound -Based Cardiac Resynchronization System in Heart Failure. JAMA Cardiol. 2024:9(10):871-879. doi:10.1001/jamacardio 2024.2050V
- Samual Chaveau, Peter R Brink, Ira S. Cohen. Stem Cell Based Biological Pacemakers From Proof of Principle to Therapy: a Review. Cytotherapy. 2014 May 13; 169&0: 873-880. doi:10.1016/j.jcyt.2014.02.014