By decoding the subtle timing of light, scientists could give surgeons sharper vision in the operating room – and patients a brighter outlook beyond it
Light has always been a guide for discovery. We have been using it to explore the Universe with telescopes, to reveal microscopic worlds with microscopes, and increasingly, to peer into the mysteries of our own bodies. In medicine, light is more than just a way to see: it can expose what is hidden, revealing details invisible to the naked eye. Furthermore, light is non-invasive, meaning that crucial information can be retrieved without damaging the target. Among the most fascinating techniques that use light, one stands out for its ability to transform cancer surgery: time-resolved fluorescence.
The fluorescence lifetime
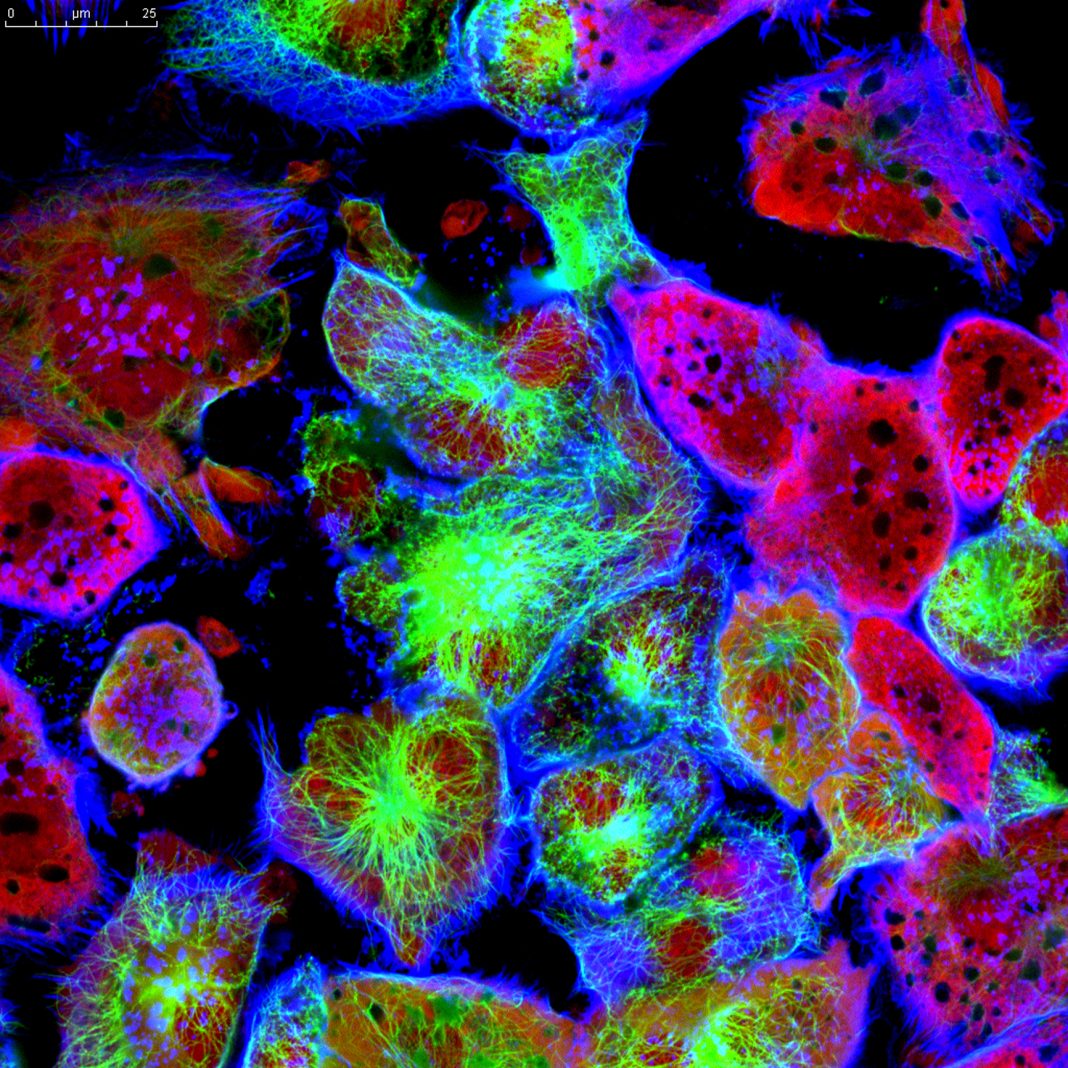
At its heart, the idea is simple yet powerful. Certain cells, when illuminated, absorb energy and re-release it as a faint glow known as fluorescence. This is due to fluorophores that naturally occur in most human tissues, such as collagen, elastin, and NADH, among others. Cancerous conditions cause a change in the way light interacts with cells, potentially altering the intensity and/or shape of the emitted fluorescence. While brightness alone can be misleading, since a tumor and the surrounding tissue may glow with similar intensity, making it difficult to distinguish where the disease ends and healthy tissue begins, the real secret lies not in how bright the glow is, but in how long it lasts.
This duration, called the fluorescence lifetime, is exquisitely sensitive to the molecular environment. Cancer cells, for example, alter their metabolism in ways that change the timing of their fluorescence. Measuring these tiny differences – on the scale of billionths of a second – creates an optical fingerprint that can distinguish malignant from healthy tissue.
If this sounds like laboratory science far removed from the hospital, the opposite is true. The operating room is precisely where this technology could make the greatest difference. When a surgeon removes a tumor, one of the hardest tasks is knowing exactly how far to cut. Too conservative, and malignant cells remain behind. Too aggressive, and vital healthy tissue is damaged. This is particularly harmful when it comes to the brain. Currently, intraoperative decisions are primarily based on visual inspection, surgical expertise, and preoperative imaging modalities. Time-resolved fluorescence can offer something more: a map generated by light itself, pointing out the tumor’s true borders.
There is, however, a catch: speed. Measuring the shape of an ultrafast fluorescence signal with such precision is not trivial, and in a laboratory, it may take minutes to gather and analyze the data. In surgery, that is unthinkable. Every second counts. A system that cannot keep up risks being ineffective, regardless of its accuracy. That is why researchers are racing to develop detectors and electronics capable of ultrafast recording of fluorescence and converting them into clear images in real-time. The aim is simple: as the surgeon moves the scalpel, the screen updates instantly, much like a GPS guiding a driver through a city.
Speed and precision of time- resolved fluorescence imaging
The benefits could be enormous. Fluorescence lifetime imaging could help ensure no malignant cells are left at the margin of a removed tumor. It could help locate sentinel lymph nodes, critical in stopping the spread of diseases like breast cancer or melanoma. It could enable doctors to distinguish tissues that appear identical to the naked eye, offering a level of precision never before available in real-time.
And the promise does not stop at surgery. Gastroenterologists could use the same principle in endoscopy to spot early-stage tumors in the digestive tract. Dermatologists might identify malignant skin lesions without resorting to invasive biopsies. Researchers are even testing it as a way to track how drugs spread through the body, using ultra-low light as a silent messenger of molecular activity.
The next step is making these systems smaller, faster, and easier to use. Surgeons cannot work with bulky laboratory setups; they require compact, reliable tools that integrate seamlessly into the flow of an operation.
In this scenario, the European Research Council (ERC), the premier European funding organisation for excellent frontier research, funded the HÈRMES project under its Starting Grant programme. Giulia Acconcia, Associate Professor at Politecnico di Milano since 2024, is the Principal Investigator of this five-year project (2024-2028) focused on making high-precision time-resolved fluorescence as fast as it has ever been. Among the techniques that can be used to carry out time-resolved fluorescent measurements, Time Correlated Single Photon Counting (TCSPC) stands out for its ability to retrieve ultrafast optical signals with superior precision. Nonetheless, it has historically been severely limited in terms of speed, as obtaining the correct signal shape without distortion was only possible by operating the acquisition instrumentation at very slow speeds. In the first phase of the HÈRMES project, Prof. Acconcia’s team demonstrated a new viable path to ultra-fast TCSPC measurements without distortion, providing both theoretical and experimental evidence. The new methodology opens the way to the exploitation of this extremely powerful tool in the most demanding scenarios of cancer surgery. A new generation of detectors, capable of combining high precision and high speed, is now necessary to make that vision realistic. Add Artificial Intelligence to the mix – algorithms capable of instantly interpreting lifetime patterns – and the surgeon could have a powerful digital assistant providing a second opinion during delicate procedures.
Time-resolved fluorescence is not just a new way of looking. It is a new way of understanding, a way to let light tell its story not only in terms of color and brightness, but also in terms of time. And in the fight against cancer, where precision can save lives, every bit of light matters. By capturing and analyzing fluorescence quickly enough, medicine may soon give surgeons a new kind of vision – one in which light itself guides the path to healing.