Dr Adèle Ehongo addresses the diagnosis of buried optic disc drusen (BODD) using Optical Coherence Tomography (OCT) and the importance of correlating visual field abnormalities and OCT data, especially in normal tension glaucoma, to distinguish it from Optic Disc Drusen (ODD)
To support the diagnosis of glaucoma, correspondence between visual field abnormalities, optic nerve head appearance, and Optical Coherence Tomography (OCT) data is essential. When considering normal tension glaucoma (the form of glaucoma with no elevated ocular pressure), it is crucial to exclude other causes that could explain the alterations in question, since visual field deficits suggestive of glaucoma are not specific to it and could reveal other conditions, such as Optic Disc Drusen (ODD).
Diagnosing Optic Disc Drusen (ODD)
ODDs are acellular deposits composed of mucopolysaccharides, calcium, and nucleic acids located at the anterior part of the optic nerve head. These deposits are suggested to result from impaired axonal calcium flow leading to extracellular calcic collections. (1) ODDs have a global prevalence of 0.9–2.4% and tend to be hereditary. (2)
ODDs are generally asymptomatic and are thus diagnosed incidentally. However, patients may experience transient visual obscuration in 10% of cases, (3) and 88.3% of patients may develop visual field defects.(4)
The diagnosis of ODDs is easy when they are obvious on ophthalmoscopy. They are then classified as visible ODDs. In this case, they present as nodular or polycyclic, blurred distortions of the optic disc rim, and the relationship to visual field defects is clinically straightforward. (5)
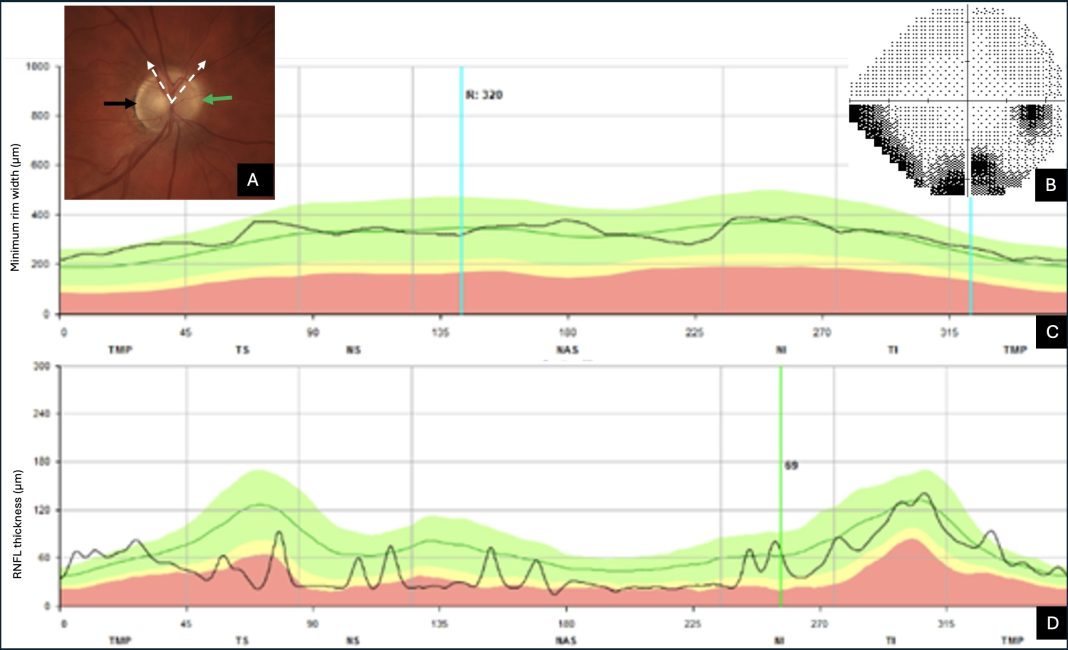
However, some ODDs are hidden within the optic nerve head and are not visible on ophthalmoscopy; these are called Buried Optic Disc Drusen (BODD). (1) In these cases, the optic nerve head has a variable appearance: normal, elevation with blurring of its margins, or even slightly pale with peripapillary atrophy (Figure 1A). BODDs may be confused with normal tension glaucoma or misdiagnosed as papilledema, leading to neuro-ophthalmologic investigations. (6)
The role of Optical Coherence Tomography (OCT)
Currently established as a standard non-invasive diagnostic tool in ophthalmology, OCT, with its latest improvements such as Swept Source-OCT and Enhanced Depth Imaging-OCT, enables the easy detection of BODDs. (7,8)
Optical Coherence Tomography device provides us with three parameters to assess glaucoma: the ganglion cell complex, the Bruch’s Membrane Opening-based Minimal Rim Width (BMO-MRW), and the Retinal Nerve Fiber Layer (RNFL) thickness.
Global and sectoral measurements of BMO-MRW and RNFL are presented as a profile curve and a classification chart. A three-color code presentation (green, yellow, red) allows the classification of a subject’s results into normal, borderline, and abnormal values, according to the OCT normative database, thus providing a rapid overview of the eye status. (9)
Typically, BMO-MRW is affected before RNFL thickness in glaucoma. Therefore, a visual field defect (Figure 1B) accompanied by an inverted presentation of this color code (Figure 1C-D) should raise concerns. Among the factors that may cause a color code discrepancy between RNFL thickness and BMO-MRW measurements (axial length, refractive errors, and vessel position), BODDs should be considered.
Radial slices centered on the optic nerve head, provided ready for use in the OCT glaucoma assessment module, reveal BODDs as round, hyporeflective lesions with hyperreflective and irregular margins. (10)
The reason why the presence of BODDs first flags abnormal RNFL measurements, while BMO-MRW is considered the most sensitive parameter, is explained by an overestimation of BMO-MRW by the added volume effect related to the presence of BODDs in the optic nerve head.
Although the alterations caused by visible ODDs on the RNFL and their impact on the visual field are well known, this association was still recently controversial for BODDs. (11, 12)
It has been assumed that BODDs are early-stage ODDs that have not yet had time to externalize and cause damage. (11) This hypothesis is supported by their age-related prevalence: BODDs are more common in children, while a transition period is described in adolescence during which BODDs would externalize. (1,13)
The impact of BODDs on Optical Coherence Tomography parameters and visual field
Using the established relationship between visual field patterns and their corresponding regions on the optic nerve head, we recently performed a study to clarify the impact of BODDs on OCT parameters and visual field. (10)
The main findings of our study are summarized below:
- BODDs don’t just affect young patients. They may also be more harmful than expected, as we observed visual field defects in 63% of cases.
- There is a correlation between BODD’s location, RNFL lesions, and the distribution of visual field defects.
- In OCT, RNFL thickness is a better parameter to assess the impact of BODDs, because the presence of BODDs in the optic nerve head leads to an overestimation of BMO-MRW, as discussed above.
- Finally, our study showed that the circumstances of BODD diagnosis were linked to glaucoma in 60% of cases: assessment of the impact of angle closure, seeking a second opinion for glaucoma diagnosis, and referral for assessment for normal tension glaucoma.
Currently recognized as a standard in ophthalmology, OCT is a valuable and cost-effective tool for ruling out the presence of BODDs. In glaucoma clinics, considering this diagnosis helps avoid unnecessary additional investigations at the slightest doubt.
References
- Allegrini D, Pagano L, Ferrara M, Borgia A, Sorrentino T, Montesano G, Angi M, Romano MR. Optic disc drusen: a systematic review: up-to-date and future perspective. Int Ophthalmol 2020;40(8):2119-2127.
- Serpen JY, Prasov L, Zein WM, Cukras CA, Cunningham D, Murphy EC, Turriff A, Brooks BP, Huryn LA. Clinical features of optic disc drusen in an ophthalmic genetics cohort. J Ophthalmol 2020;2020:5082706.
- Ahmed H, Khazaeni L. Optic Disc Drusen. In: StatPearls. Treasure Island (Florida): StatPearls Publishing; 2022.
- Sustronck P, Nguyen DT, Jean-Charles A, David T, Merle H. Visual field defects due to optic nerve drusen in Afro-Caribbean patients: a case series of 16 eyes. J Fr Ophtalmol 2021;44(7):989-994.
- Wilkins JM, Pomeranz HD. Visual manifestations of visible and buried optic disc drusen. J Neuroophthalmol 2004;24(2):125-129.
- Razek AAKA, Batouty N, Fathy W, Bassiouny R. Diffusion tensor imaging of the optic disc in idiopathic intracranial hypertension.Neuroradiology 2018;60(11):1159-1166.
- Gise R, Gaier ED, Heidary G. Diagnosis and imaging of optic nerve head drusen. Semin Ophthalmol 2019;34(4):256-263.
- Guo XH, Wu YJ, Wu YH, Liu H, Ming S, Cui HP, Fan K, Li SY, Lei B. Detection of superficial and buried optic disc drusen with swept-source optical coherence tomography. BMC Ophthalmol 2022;22(1):219.
- La Bruna S, Tsamis E, Zemborain ZZ, Wu Z, De Moraes CG, Ritch R, et al. A Topographic Comparison of OCT Minimum Rim Width (BMO-MRW) and Circumpapillary Retinal Nerve Fiber Layer (cRNFL) Thickness Measures in Eyes With or Suspected Glaucoma. J Glaucoma. 2020 Aug;29(8):671–8
- Nana Wandji B, Dugauquier A, Ehongo A. Visual field defects and retinal nerve fiber layer damage in buried optic disc drusen: a new insight. Int J Ophthalmol. 2022 Oct 18;15(10):1641-1649. doi: 10.18240/ijo.2022.10.12. PMID: 36262850; PMCID: PMC9522567.
- Malmqvist L, Wegener M, Sander BA, Hamann S. Peripapillary retinal nerve fiber layer thickness corresponds to drusen location and extent of visual field defects in superficial and buried optic disc drusen. J Neuroophthalmol 2016;36(1):41-45.
- Katz BJ, Pomeranz HD. Visual field defects and retinal nerve fiber layer defects in eyes with buried optic nerve drusen. Am J Ophthalmol 2006;141(2):248-253.e1.
- Hamann S, Malmqvist L, Costello F. Optic disc drusen: understanding an old problem from a new perspective. Acta Ophthalmol 2018;96(7): 673-684.