Recompensation in liver disease indicates both a physical and molecular improvement in liver functions. Molecular regeneration is key to improving liver function, and novel technologies in proteomics and RNA transcriptomics may hold the key to advancing liver regeneration in alcohol-related liver disease. Nina Kimer explains
We need a larger focus on the integration of treatments for alcohol use disorder in hepatology clinics. Future research on molecular and cellular regeneration mechanisms in the liver is highly warranted in liver cirrhosis, an area where novel omics technologies and RNA transcriptomics may be quite helpful. Integrating translational research with the clinical application of novel diagnostic, prognostic, and monitoring markers for liver regeneration, even in advanced liver disease, is warranted.
Recompensation of liver cirrhosis
Alcohol related liver disease is ever- present in the healthcare systems across Europe, and the economic and social burden on hospitals and families is substantial. In recent years, the clinical term ‘recompensation’ has emerged in liver disease, indicating the removal of the disease-causing factor and an improvement in clinical symptoms and liver function, to a degree that patients are free from frequent hospital admissions and even medication. (1) This stage is highly desirable, as it is associated with a markedly improved prognosis, better quality of life, and an increase in quality-adjusted life years.
Treatment of alcohol use disorder in advanced liver disease
In alcohol related liver cirrhosis, a removal of the cause means complete abstinence from alcohol. Although efficient treatment with motivational enhancement therapy and cognitive behavioral therapy is practiced for alcohol use disorder, these therapeutic aspects are not implemented in the clinical practice of hepatology. Misconceptions and perceptions of both alcohol use and cognitive therapy are barriers to effective treatment of alcohol use disorder in advanced cirrhosis. Medical drug therapy for alcohol use disorder in liver cirrhosis is limited. Naltrexone and acamprosate are cost-effective in terms of preventing admissions to hospital in patients with alcohol related cirrhosis, but in fact, we do not have high-quality randomized trials of any drugs for alcohol use disorder in patients with cirrhosis.
The best-case scenario on alcohol related liver disease is a remission from physical symptoms and a restoration of liver function to a level where the patients can live a life as close to normal as possible.
Restoration of liver functions
The definition of recompensation also includes a restoration of hepatic synthesis. Hepatic synthesis is not a single mechanism of action, but rather a variety of cells in the liver expressing various biomarkers and pathways involved in protein synthesis, biomarker production, and activation of pathways, all involved in the regeneration of liver tissue.
Several cellular mechanisms are involved in inflammation, apoptosis, and fibrosis when the liver is affected by harmful substances.
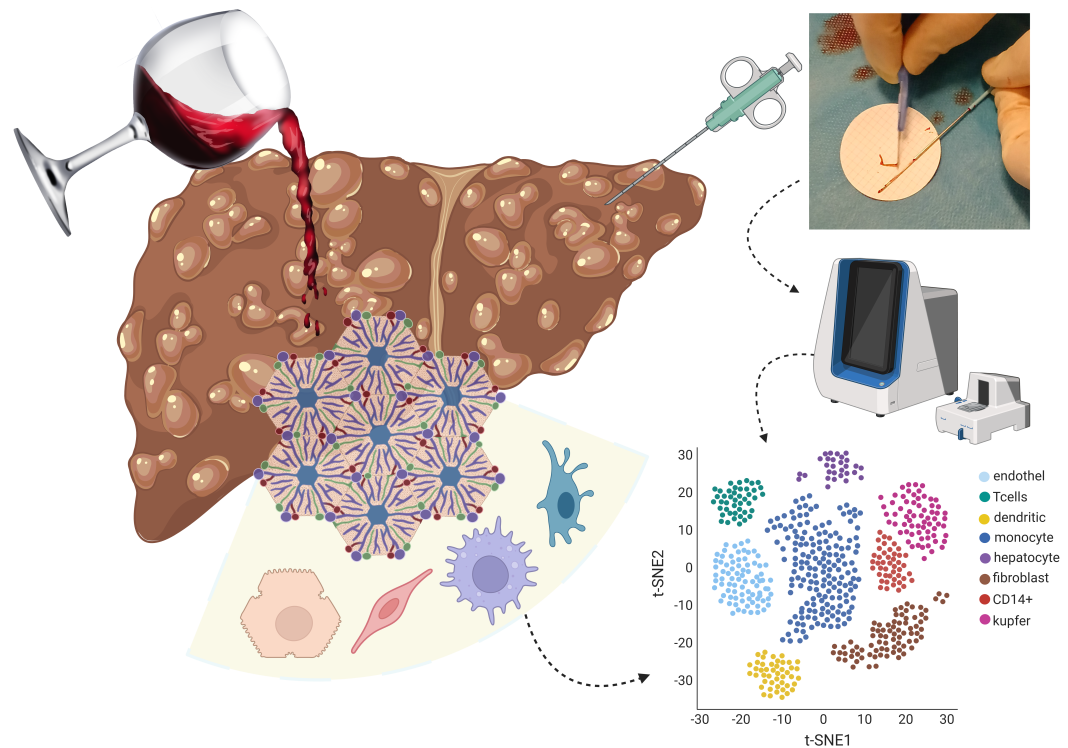
Various biomarkers, cytokines, and pathways are investigated in liver regeneration; some are directly involved in liver regeneration, some are antagonists of liver damage and inflammation. Most studies are performed in mice and are not directly applicable to humans. Granulocyte colony-stimulating factor has shown promising results in liver regeneration as an enhancer of responsiveness to prednisolone in alcohol related hepatitis; the potential in chronic liver cirrhosis is unknown. (2) Alas, no treatment facilitates liver generation, yet there is a huge potential for studying regeneration mechanisms in various compounds of the liver, the regenerative nodules, endothelial cells, Kupfer cells and there is also potential of reversing fibrosis even in patients with advanced liver disease.
Translational studies of liver regeneration
A large proportion of people diagnosed with alcohol related liver cirrhosis have advanced disease and complications at the time of diagnosis. These people are key to understanding liver regeneration in the clinical course of disease, improvement, and regression of disease. Large, prospective cohort studies, longitudinal data collection, and novel technologies may be the cocktail that breaks the code of liver regeneration in the future. Full- spectrum proteomics and lipidomics now map the entire spectrum of biomarkers in the liver, and a proteomic fingerprint of liver regeneration can be identified and compared with the clinical presentation of remission, even in alcohol-related liver disease. Single- cell RNA sequencing allows us to study mechanisms of action in the remission of cirrhosis over time. (3) We might be able to identify molecular predictors of regeneration and recompensation that align with the clinical presentation, or even molecular pathways that could serve as novel drug targets in the future.
References
- Recompensation in decompensated cirrhosis. Madhumita Premkumar, Patrick S Kamath, Thomas Reiberger, K Rajender Reddy. Lancet Gastroenterol Hepatol 2025;10:1028-40. doi: https://doi.org/10.1016/S2468-1253(25)00095-0
- Granulocyte Colony-Stimulating Factor Improves Prednisolone Responsiveness and 90-Day Survival in Steroid-Eligible Severe Alcohol-Associated Hepatitis: The GPreAH Study, a Randomized Trial. Ajay Kumar Mishra, Saggere Muralikrishna Shasthry, Rajan Vijayaraghavan, Guresh Kumar, Shiv K Sarin. Am J Gastroenterol. 2025 May 1;120(5):1087-1097. doi: https://doi.org/10.14309/ajg.0000000000003038
- Longitudinal paired liver biopsies and transcriptome profiling in alcohol-associated hepatitis reveal dynamic changes in cellular senescence. Daniel Rodrigo-Torres, Alastair M Kilpatrick, Sofia Ferreira-Gonzalez, Rhona E Aird, Stephen Rahul Atkinson, Victoria L Gadd, et al. Gut. 2025 Aug 7;74(9):1500-1513. doi: https://doi.org/10.1136/gutjnl-2024-334094.