Professor Nicholas Harvey, President of the International Osteoporosis Foundation, posits the urgent need to address the burden of bone health and the associated chronic conditions, which are putting immense strain on public health and health services
Every minute, 70 fractures occur in people aged over 55 because of fragile bones – yet most will never be tested or treated for osteoporosis, the disease that causes the break. Despite advances in diagnosis and therapy, this common but silent condition remains dangerously underrecognized and undertreated, leaving millions at risk of preventable disability and premature death.
A silent epidemic on the rise
Osteoporosis is among the most common chronic diseases, affecting an estimated 500 million people worldwide. One in three women and one in five men over the age of 50 will experience an osteoporosis-related fracture in their remaining lifetimes. As populations age, the number of fractures each year is expected to double in some regions of the world, placing an immense strain on healthcare systems.
The consequences go far beyond the initial injury. Fractures can rob people of independence, forcing them to rely on family or long-term care. In many countries, up to 24% of hip fracture patients die within a year of their injury. The human cost – along with the growing financial burden of hospitalization, rehabilitation, and the need for long-term care – is staggering.
Out of sight, out of mind
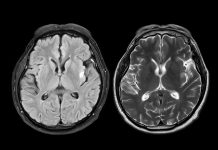
One reason bone health is so often neglected is that bone loss is invisible. You can’t see or feel your bones thinning, and without obvious symptoms, both patients and doctors may underestimate the risk. Routine check-ups typically focus on heart and metabolic health, including blood pressure, cholesterol, and blood sugar levels, while assessments of bone density and fracture risk are often overlooked.
Osteoporosis is often discovered only after a fracture has occurred. Yet up to 80% of patients who suffer these fragility fractures never receive follow-up testing or treatment to reduce the risk of breaking another bone. This care gap stems from factors such as a lack of awareness among both healthcare professionals and the general public, inadequate resources and prioritization, and broader systemic barriers.
Closing the care gap: the need for systemic change
The International Osteoporosis Foundation (IOF) recently released a Position Paper highlighting critical barriers to care and calling for urgent global action to improve fracture prevention. Similarly, the 2025 World Osteoporosis Day campaign highlighted the ongoing and unacceptable neglect of bone health.
Work from the IOF has demonstrated that despite advances in assessment and treatment, most patients at high risk of fracture still do not receive appropriate care, particularly in under-resourced regions of the world, but also in affluent regions such as Europe. The IOF SCOPE21 study of 29 European countries found that on average, 71% of women who were eligible for treatment remained untreated.
Multiple factors contribute to this care gap, including limited access to bone density scanning (DXA), outdated treatment criteria that rely solely on bone mineral density, and uncertainty over when intervention is warranted. Even when a patient is judged to require treatment, financial and administrative barriers – such as restrictive reimbursement policies for scans and medications – can impede both physician prescribing and patient adherence, further impacted by misplaced concerns over serious but very rare side effects.
For those who have experienced a fragility fracture, Fracture Liaison Services (FLS) – specialized hospital-based programmes that identify fracture patients, connect them to osteoporosis care, and coordinate long-term follow-up. Although the number of FLS programmes is growing, they remain scarce in most health systems. Without such services, patients often ‘fall through the cracks,’ receiving orthopaedic repair but no treatment for the disease that caused the fracture. The result is a revolving door of repeat fractures, rising healthcare costs, and avoidable suffering.
However, FLS does not address the prevention of a first fracture. The IOF therefore emphasises the urgent implementation of effective mechanisms worldwide to ensure that every individual at high fracture risk is appropriately assessed and treated. The IOF proposes that the focus should be on detecting high fracture risk using established fracture risk calculators, such as FRAX®, incorporating bone mineral density measures when available. In this way, treatment does not rely solely on the availability of bone density scanning or the diagnosis of osteoporosis, but rather on a validated measure of fracture risk, which is already established as an indication for therapy.
Coordinated action urgently needed
Osteoporosis is a silent epidemic, but its effects are anything but quiet. To make real progress, countries must adopt comprehensive bone health strategies – updating reimbursement policies to focus on individualised absolute fracture risk, supporting FLS programmes, and integrating routine bone assessments into standard preventive care for older adults or those with risk factors. Public awareness campaigns can help people understand that strong bones, nurtured from youth through older age, are as vital as a healthy heart.
Until bone health receives the attention it deserves, the global crisis of fragility fractures will continue to grow. Early detection, equitable access to care, and coordinated follow-up could transform outcomes for millions – making this hidden crisis entirely preventable.