Oliver Bathe from the University of Calgary and Qualisure Diagnostics, walks us through addressing the surge in papillary thyroid cancer incidence by refining cancer care through molecular diagnostics
The incidence of papillary thyroid cancer (PTC) is rising by more than 6% in most developed countries, mainly due to increased early detection. While early detection is generally beneficial in cancer care, PTC presents a unique challenge. Because it is rarely life-threatening, the discovery of small, early-stage tumors raises the question of how to manage them without causing harm through overtreatment.
It is well established that many patients with PTC receive more aggressive care than necessary, including total thyroidectomy, radioactive iodine (RAI), and prolonged follow-up after treatment. This overtreatment stems from the difficulty of predicting recurrence risk before treatment begins. At the heart of the issue is the absence of accurate and timely prognostic tools.
A new molecular test, Thyroid GuidePx®, was developed to fill this gap. This test evaluates the biological behavior of a PTC tumor before treatment decisions are made. Through advanced transcriptomic analysis, it provides an individualized prediction of recurrence risk, enabling patients and clinicians to tailor treatment appropriately – and avoid unnecessary intervention when a less intensive approach is safe.
Understanding the science behind Thyroid GuidePx®
The test is based on transcriptomics, a field of molecular biology that examines RNA, the molecule that carries out the instructions coded in a cancer’s DNA. While DNA mutations can tell us what might go wrong in a tumor, RNA tells us what is currently happening. It shows which genes are turned on or off, revealing the biological processes driving tumor behavior in real-time. In other words, transcriptomics provides a functional snapshot of a tumor’s activity.
In thyroid cancer, this distinction is critical. DNA-based tests, which look for mutations like BRAF or TERT, have been used for many years. But their predictive value is limited. BRAF mutations are found in over half of all PTC cases, including many low-risk tumors. TERT mutations are more strongly associated with recurrence; however, they are relatively uncommon and often need to be interpreted in context. Neither mutation alone can offer a clear prognosis.
Thyroid GuidePx® takes a different approach. Rather than focusing on one or two mutations, it analyzes the expression levels of genes most closely related to recurrence risk.
This approach captures the complex interplay of genetic, epigenetic, and regulatory factors that shape how the tumor behaves. By applying machine learning techniques to large datasets of patients with known outcomes, researchers identified a specific gene expression pattern that correlates strongly with recurrence risk.
How the test was developed and validated
The development of Thyroid GuidePx® involved an international collaboration that brought together patient data from North America and Asia. Researchers used RNA sequencing to measure gene activity in hundreds of thyroid tumors, then trained a machine learning model to identify patterns associated with structural recurrence – the return of cancer in the neck or other parts of the body after initial treatment.
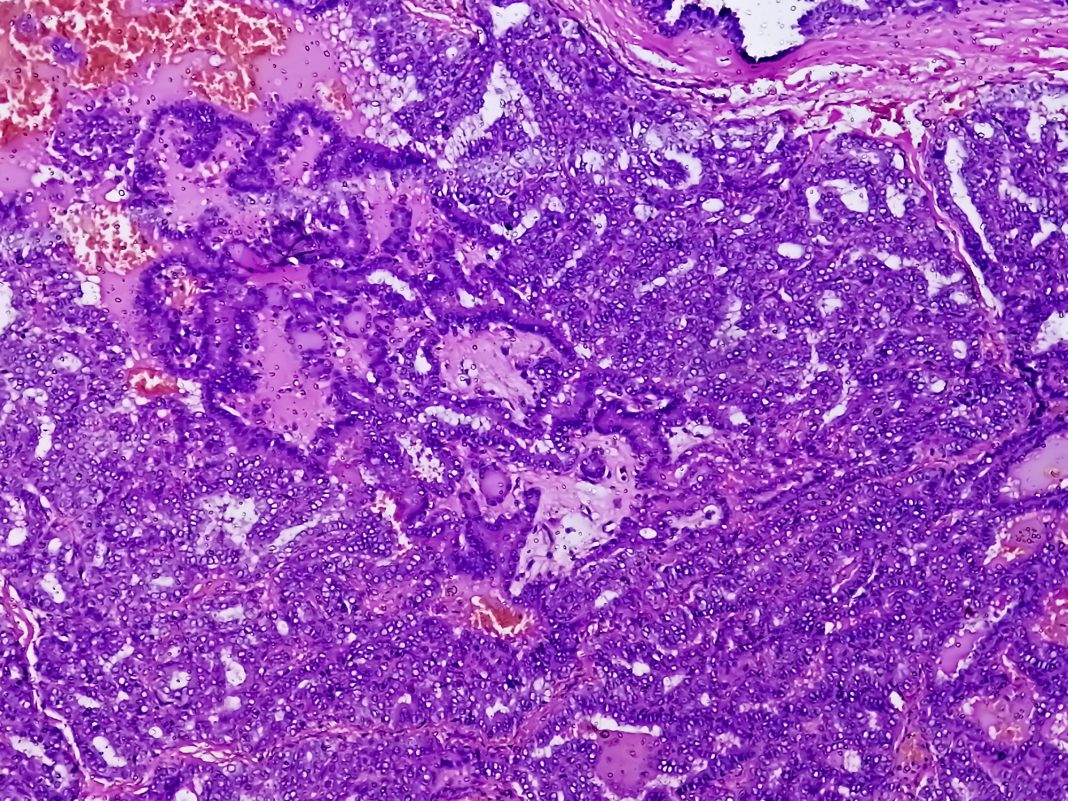
This analysis revealed three distinct molecular subtypes of PTC. Type 1 tumors were well-differentiated, slow-growing, and rarely recurred. Type 3 tumors showed signs of biological aggressiveness, including features like dedifferentiation and immune suppression. These tumors had high rates of recurrence, even when they were small and early-stage. Type 2 tumors fell in between, sharing some clinical features with Type 3, but with much lower recurrence rates.
The model was then tested in three independent patient cohorts from the United States, Canada, and South Korea. In each of these populations, the molecular classification outperformed traditional risk assessment tools, including the widely used American Thyroid Association (ATA) system. The test accurately identified high-risk tumors that might otherwise have been misclassified, and it helped distinguish truly low-risk cancers from those with uncertain features.
What the test measures and what it tells us
Thyroid GuidePx® measures the expression of 82 genes. The gene expression pattern determines the molecular subtype, which is the most powerful determinant of recurrence risk. This information is delivered in a format that physicians can use during the decision-making process, typically before surgery or shortly afterward.
The ability to assign risk preoperatively is particularly important. Most existing prognostic tools rely on information that is only available after surgery – such as the tumor’s appearance under the microscope, its growth pattern, or the presence of vascular invasion. But by that point, many patients have already undergone a total thyroidectomy or begun planning for radioactive iodine treatment.
Thyroid GuidePx® shifts the timing of risk assessment to an earlier stage. When the test indicates a low-risk Type 1 tumor, the surgeon and patient may feel more confident choosing a lobectomy rather than removing the entire thyroid. If the result shows a high-risk Type 3 tumor, the team may opt for a total thyroidectomy and closer follow-up. The test thus plays a central role in shaping treatment decisions before irreversible steps are taken.
Why this approach matters in clinical practice
The implications of this test go far beyond academic interest. In real-world practice, physicians are often confronted with difficult trade-offs. Patients want reassurance that their treatment plan is appropriate, and they want to avoid overtreatment if possible. At the same time, doctors are understandably cautious about underestimating risk, especially in the absence of definitive data.
Thyroid GuidePx® provides that missing information. By anchoring treatment decisions in tumor biology rather than general assumptions, the test helps avoid unnecessary procedures while still protecting patients who genuinely need aggressive care. For example, patients with small tumors might otherwise be considered for a partial thyroidectomy or active surveillance. Radiofrequency ablation may be an option. But without molecular data, these options can feel risky. Thyroid GuidePx® can identify which tumors are biologically quiet and therefore safe to monitor – and which are not.
The test also improves the clarity of discussions between doctors and patients. Instead of relying on uncertain estimates or retrospective guidelines, physicians can point to specific molecular evidence to justify a recommended course of action. This makes shared decision-making more informed and more collaborative.
Building toward more personalized cancer care
Thyroid GuidePx® reflects a broader shift in oncology: the move from one-size-fits-all treatment to personalized care based on the unique characteristics of each patient’s tumor.
In thyroid cancer, this shift is overdue. For too long, treatment decisions have been driven by tumor size, anatomical spread, and subjective pathology reports. While these factors are important, they do not fully capture the biology that drives recurrence.
With the integration of transcriptomics, thyroid cancer care can finally join other areas of oncology that have embraced molecular profiling. Tools like Thyroid GuidePx® represent a more modern, biologically grounded approach to prognostication – one that respects the complexity of the disease and the individuality of each patient.