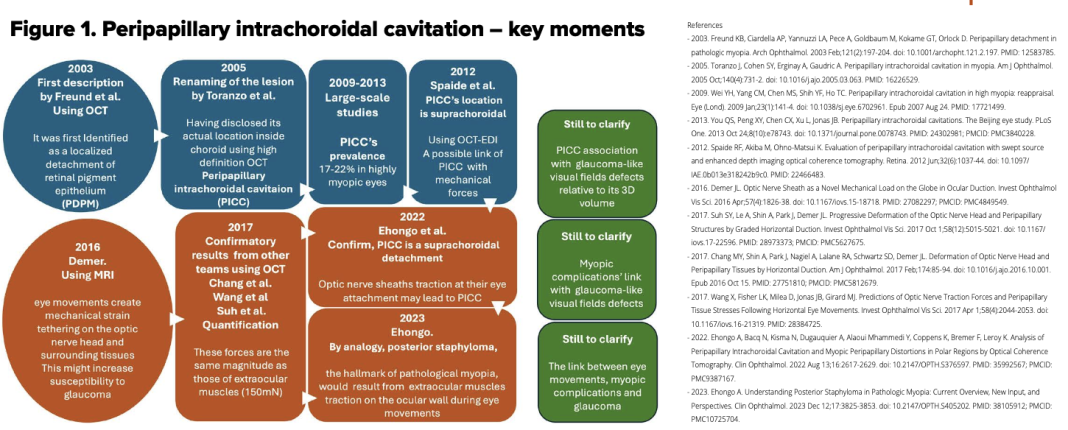
Dr Adèle Ehongo discusses Peripapillary intrachoroidal cavitation and biomechanical considerations in a multi-stage narrative
The clinical relevance of disclosing Peripapillary intrachoroidal cavitation
Peripapillary intrachoroidal cavitation is a complication of highly myopic eyes found in up to 22% of cases. It is a well-circumscribed yellow-orange lesion located at the outer border of the myopic conus. However, this aspect may be absent in half of the cases of Peripapillary intrachoroidal cavitations. (1) This myopic complication is related to visual field defects mimicking those of glaucoma. (2) Diagnosing this entity is more clinically relevant than ever since forecasts predict that 50% of people will be myopic by 2050. (3)
The peripapillary zone, the site of several changes in myopic eyes
The condition is associated with posterior staphyloma and gamma peripapillary atrophy, two other myopic changes. As these entities often coexist in myopic eyes, we conducted a study that showed that Peripapillary intrachoroidal cavitation is present only in eyes combining peripapillary staphyloma and gamma peripapillary atrophy. (4) However, less than 25% of eyes with this combination exhibited a Peripapillary intrachoroidal cavitation (4), which raises the question of what factors predispose some eyes to develop Peripapillary intrachoroidal cavitation.
The structural substrate of the Peripapillary intrachoroidal cavitation: A suprachoroidal detachment
To clarify this question, we conducted a second study exploring the deep polar peripapillary regions of eyes, combining peripapillary staphyloma and gamma peripapillary atrophy. (5) Advances in optical coherence tomography had already revealed that Peripapillary intrachoroidal cavitation is a hyporeflective intrachoroidal thickening with little or no deformation of the overlying plane of Bruch’s membrane. (6) Our results established that Peripapillary intrachoroidal cavitation is, in fact, a suprachoroidal detachment (5), which has been previously suggested. (6)
Peripapillary intrachoroidal cavitation and eye motions Peripapillary changes associated with Peripapillary intrachoroidal cavitation (4), along with previous biomechanical results (7), led us to suggest that Peripapillary intrachoroidal cavitation might result from repetitive tractions exerted by the optic nerve sheaths at their scleral attachment during adduction. (5) The same mechanism has previously been suggested for tilted disc (7,8) and would promote the peripapillary staphyloma. (5) This highlights the clinical relevance of the involved forces, whose magnitude is the same as that of the extraocular muscles. (9) However, these tractions occur in all individuals, raising the question of why Peripapillary intrachoroidal cavitation only affects a minority of eyes.
More severe peripapillary deformations in eyes with Peripapillary intrachoroidal cavitation
In a step forward, we found that among eyes with a combination of peripapillary staphyloma and gamma peripapillary atrophy, visual field defects were significantly more common in the subgroup of eyes with Peripapillary intrachoroidal cavitation. (2)
Furthermore, through multivariate logistic regression analysis, we showed that the only factor discriminating between the two subgroups was the ovality index (2) (the ratio between the shortest and longest diameters of the disc), which reflects the severity of the optic disc tilt. This ovality index was lower in the subgroup with Peripapillary intrachoroidal cavitation, meaning that the optic nerve head in this subgroup was significantly more deformed.
Another myopic complication and eye motions
Myopic complications like peripapillary staphyloma and Peripapillary intrachoroidal cavitation were then suggested to result from long-term remodelling and fixation of intermittent eyewall deformations induced by optic nerve sheaths on their scleral attachments during eye movements. (5) Since the magnitude of the pulling forces involved reaches that of the extraocular muscles (7,9), similarities have been established for posterior staphyloma, a hallmark of pathologic myopia. (10) The oblique muscles, which also insert at the back of the eyeball, could potentially promote the development of other types of posterior staphylomas through the same mechanism. (10) This warrants further investigation.
Future directions
The question remains why eyes with Peripapillary intrachoroidal cavitation predominantly exhibit more deformations leading to visual field defects? Either the traction forces are stronger in these eyes, or the biomechanical properties of eyes with Peripapillary intrachoroidal cavitation make them more sensitive to the forces deployed. Interestingly, finite elements modelling has shown that stiff meningeal sheaths or soft sclera are associated with more peripapillary deformations. (9) These questions warrant further investigation.
It would also be interesting to compare the biomechanical properties of eyes with Peripapillary intrachoroidal cavitation to those without Peripapillary intrachoroidal cavitation.
Myopia health: Conclusion
Currently, myopia and its complications constitute a public health problem that mobilises the scientific community. Interestingly, various aspects are being considered, from prevention to the treatment of complications, to reduce the burden of myopia in the future.
References
- Ehongo A, Bacq N. Peripapillary Intrachoroidal Cavitation. J Clin Med. 2023 Jul 16;12(14):4712. doi: https://doi.org/10.3390/jcm12144712. PMID: 37510829; PMCID: PMC10380777.
- Ehongo A, Dugauquier A, Kisma N, De Maertelaer V, Nana Wandji B, Tchatchou Tomy W, Alaoui Mhammedi Y, Coppens K, Leroy K, Bremer F. Myopic (Peri)papillary Changes and Visual Field Defects. Clin Ophthalmol. 2023 Nov 1;17:3295-3306. doi: https://doi.org/10.2147/OPTH.S404167. PMID: 37933329; PMCID: PMC10625749.
- Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016 May;123(5):1036-42. doi: https://doi.org/10.1016/j.ophtha.2016.01.006. Epub 2016 Feb 11. PMID: 26875007.
- Ehongo A, Hasnaoui Z, Kisma N, Alaoui Mhammedi Y, Dugauquier A, Coppens K, Wellens E, de Maertelaere V, Bremer F, Leroy K. Peripapillary intrachoroidal cavitation at the crossroads of peripapillary myopic changes. Int J Ophthalmol. 2023 Dec 18;16(12):2063-2070. doi: https://doi.org/10.18240/ijo.2023.12.20. PMID: 38111938; PMCID: PMC10700091.
- Ehongo A, Bacq N, Kisma N, Dugauquier A, Alaoui Mhammedi Y, Coppens K, Bremer F, Leroy K. Analysis of Peripapillary Intrachoroidal Cavitation and Myopic Peripapillary Distortions in Polar Regions by Optical Coherence Tomography. Clin Ophthalmol. 2022 Aug 13;16:2617-2629. doi: https://doi.org/10.2147/OPTH.S376597. PMID: 35992567; PMCID: PMC9387167.
- Spaide RF, Akiba M, Ohno-Matsui K. Evaluation of peripapillary intrachoroidal cavitation with swept source and enhanced depth imaging optical coherence tomography. Retina. 2012;32(6):1037–1044. doi:https://doi.org/10.1097/IAE.0b013e318242b9c0
- Wang X, Beotra MR, Tun TA, Baskaran M, Perera S, Aung T, Strouthidis NG, Milea D, Girard MJ. In Vivo 3-Dimensional Strain Mapping Confirms Large Optic Nerve Head Deformations Following Horizontal Eye Movements. Invest Ophthalmol Vis Sci. 2016 Oct 1;57(13):5825-5833. doi: https://doi.org/10.1167/iovs.16-20560. PMID: 27802488.
- Chang MY, Shin A, Park J, Nagiel A, Lalane RA, Schwartz SD, Demer JL. Deformation of Optic Nerve Head and Peripapillary Tissues by Horizontal Duction. Am J Ophthalmol. 2017 Feb;174:85-94. doi: https://doi.org/10.1016/j.ajo.2016.10.001. Epub 2016 Oct 15. PMID: 27751810; PMCID: PMC5812679.
- Wang X, Fisher LK, Milea D, Jonas JB, Girard MJ. Predictions of Optic Nerve Traction Forces and Peripapillary Tissue Stresses Following Horizontal Eye Movements. Invest Ophthalmol Vis Sci. 2017;58(4):2044– 2053. PMID: 28384725. doi:https://doi.org/10.1167/iovs.16-21319.
- Ehongo A. Understanding Posterior Staphyloma in Pathologic Myopia: Current Overview, New Input, and Perspectives. Clin Ophthalmol. 2023 Dec 12;17:3825- 3853. doi: https://doi.org/10.2147/OPTH.S405202. PMID: 38105912; PMCID: PMC10725704.