Fredric Gorin, Sarah Torres, and Pamela J. Lein discuss the implications of vitamin A supplementation during a recent measles outbreak in the US. They explain that a common misconception – that vitamin A supplementation can prevent the transmission of measles among unvaccinated individuals – can result in vitamin A toxicity
Vitamin A has garnered recent media attention as a preventative for measles, an interest driven in large part by reports in 2025 of the first major outbreak of measles in the United States in more than 20 years. Worldwide, measles cases are increasing and remain one of the most serious causes of childhood morbidity and mortality. Thus far, in 2025, 21% of children in the US younger than age five years were hospitalized with measles, with an overall mortality risk of one in three out of 1,000 people. This outbreak is largely a result of reduced measles vaccination coverage.
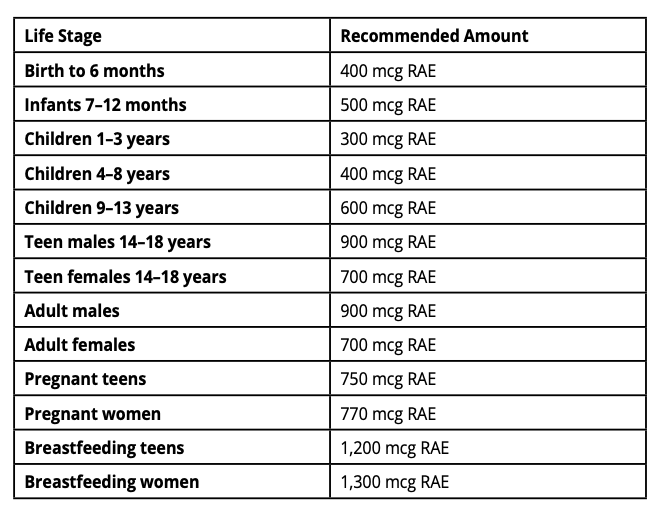
Advocacy of vitamin A supplementation for measles prevention by unvaccinated populations is based in part on two studies indicating that age-appropriate supplementation of vitamin A (see Box 1) reduced the morbidity of measles for young children under the age of five. One of these studies was from India, and the other was from Sub-Saharan Africa, both countries where vitamin A deficiency, as well as overall nutritional deficiency, is prevalent. In countries with persistent food insecurity, nutritional deficiency of vitamin A in children and pregnant women is associated with developmental, ophthalmic, and dermatological disorders. In addition, COVID-19 increased public awareness that vitamin A deficiency can also impair the host immune response to viral infections and can blunt immune responses to antiviral vaccinations.
The international studies identifying the beneficial effects of vitamin A supplementation have led to misunderstanding amongst some unvaccinated groups that vitamin A supplementation can prevent measles transmission. Unfortunately, this has led to cases of hospitalized, unvaccinated, measles patients demonstrating signs of vitamin A toxicity. While 20% of the world’s population is deficient in vitamin A, the 2017-2018 United States National Health and Nutrition Examination Survey found that less than 1% of the US population was vitamin A deficient, as defined by serum retinol levels (see Box 1). This is because many foods available in the US are enriched with vitamin A. Vitamin A supplementation in individuals who are not vitamin A-deficient can result in vitamin A toxicity because this vitamin is fat-soluble and accumulates in fat tissue.
Vitamin A toxicity
It is not generally recognized that excessive vitamin A supplementation can be toxic. Vitamin A toxicity can result from either acute or chronic overdosing. With repeated doses, vitamin A can accumulate in the body, leading to toxicity within days to weeks after taking very high amounts of vitamin A, which is 100 times the recommended daily allowance (RDA). This toxicity most often occurs from ingestion of preformed vitamin A, retinol, and retinyl esters, or more rarely from topical absorption of synthetic derivatives of retinol used medically to treat a variety of skin conditions and specific types of cancer. In contrast, consumption of foods high in vitamin A rarely causes vitamin A toxicity because the biochemical conversion of plant provitamin A carotenoids to vitamin A is relatively inefficient. Similarly, absorption of retinol and its derivatives as a cosmetic skin product is low and rarely leads to clinical symptomatology.
Young children, because of their small size, and pregnant women are at most risk for vitamin A toxicity. Acute and chronic vitamin A toxicity in pregnant women within the first trimester can cause serious fetal skeletal, cardiac, urinary tract malformations, and neurological abnormalities, including increased intracranial pressure. Acute pediatric vitamin A toxicity can be more serious with neurological consequences because children and young adults are more prone than adults to develop increased brain pressure. Acute adult vitamin A intoxication can cause nausea, vomiting, headache, elevated liver enzymes, triglycerides, and, in severe cases, liver damage.
Chronic vitamin A toxicity occurs rarely through the ingestion of animal-based foods, exceptions being excessive liver consumption or high-dose vitamin A supplements. Liver damage, renal dysfunction, hypothyroidism, and elevated triglycerides can occur, and skeletal remodeling in adults and children is associated with joint pain, fractures, and high serum levels of calcium. Symptoms can include nausea, vomiting, and persistent headaches, as well as visual loss, when associated with elevated intracranial pressure.
Measles prevention
In the US, the Centers for Disease Control and Prevention (CDC) recommends measles vaccinations at 12-15 months and again at 4-6 years of age. Age-appropriate vitamin A supplementation is recommended for nutritionally at-risk populations to enhance vaccine efficacy, but as indicated above, this recommendation for vitamin A supplementation is relevant for less than 1% of the US population. The recommended two doses of vaccination for measles are reported to be 97% effective at preventing measles transmission and reducing morbidity and mortality; in contrast, vitamin A alone does not reliably prevent measles transmission.
In summary, in individuals with vitamin A deficiency, supplementation with vitamin A will enhance the effectiveness of measles vaccinations, but even in these cases, vitamin A supplementation alone will not prevent measles. In individuals who are not deficient in vitamin A, which includes most of the population in the US and other developed countries, vitamin A supplementation can result in serious adverse health effects.
Vitamins are essential dietary nutrients required for normal health. Vitamin A is a fat-soluble vitamin enriched in specific animal tissues as retinoids and retinal esters. Plants that contain carotenoids include colorful fruits and vegetables. Carotenoids are pro-vitamin A plant pigments and include: beta-carotene, alpha- carotene, and beta-cryptoxanthin. Carotenoids require conversion to retinol primarily in the intestines, liver, and the eye’s retina. Conversion of carotenoids to retinol is relatively inefficient, and the body regulates the metabolic conversion based upon vitamin A levels; thus, vitamin A toxicity from carotenoids is extremely uncommon.


