Dr. Rob Sillevis pioneers Superficial Neuromodulation® with Magnetic Tape®, a groundbreaking non-invasive therapy. This research synthesizes years of clinical and laboratory findings, demonstrating how this simple yet scientifically profound tool can transform pain modulation, functional rehabilitation, and nervous system regulation
Introduction
Dr. Rob Sillevis, an associate professor in the Department of Rehabilitation Sciences at Florida Gulf Coast University and a researcher in the application of magnetic technology in physiotherapy. He has led a groundbreaking body of research into the use of Magnetic Tape® for pain modulation, functional rehabilitation, and nervous system regulation. With a passion for advancing non-invasive therapeutic interventions, Dr. Sillevis has brought forward an emerging concept, developed by Dr. Fransisco Selva-Sarzo, in modern rehabilitation: Superficial Neuromodulation®. This article synthesizes years of clinical and laboratory research, presenting both the science and the real-world applications of Magnetic Tape®. The goal is to make this work accessible and informative for healthcare providers, patients, educators, and the broader public interested in the future of therapeutic technology.
What follows is an exploration of the mechanisms, findings, patient outcomes, and broader implications of Magnetic Tape® research, demonstrating how a simple tool, when rooted in deep scientific understanding, can transform the approach to pain and recovery in clinical practice.
1. The science of skin and Superficial Neuromodulation
The skin is the largest organ in the human body and plays a far more dynamic role than traditionally assumed. While commonly recognized as a barrier and sensory surface, the epidermis is now understood to function in neuro-immune signaling, homeostasis regulation, and systemic communication with the brain and internal organs. Keratinocytes, the dominant cell type in the epidermis, are responsive to mechanical, thermal, and electromagnetic stimuli. They interact with peripheral nerve endings, suggesting that interventions targeting the skin can have effects that extend beyond the local application site.
Superficial Neuromodulation® is based on this understanding. It is a therapeutic concept whereby specific epidermal zones are stimulated, mechanically or electromagnetically, to influence neurological pathways. This method integrates sensory biology, segmental neuroanatomy, and functional rehabilitation strategies. Dr. Sillevis’s work connects clinical outcomes to precise biological underpinnings, bridging the gap between tactile application and systemic effect.
Unlike invasive neuromodulation techniques that require electrical implants or surgical procedures, Superficial Neuromodulation® offers a non-invasive, cost-effective, and highly accessible alternative. Magnetic Tape® becomes a tool for constant stimulation, acting on the skin for hours or days after application and triggering cascading responses within the body.
2. Magnetic Tape®: What it is and how it works
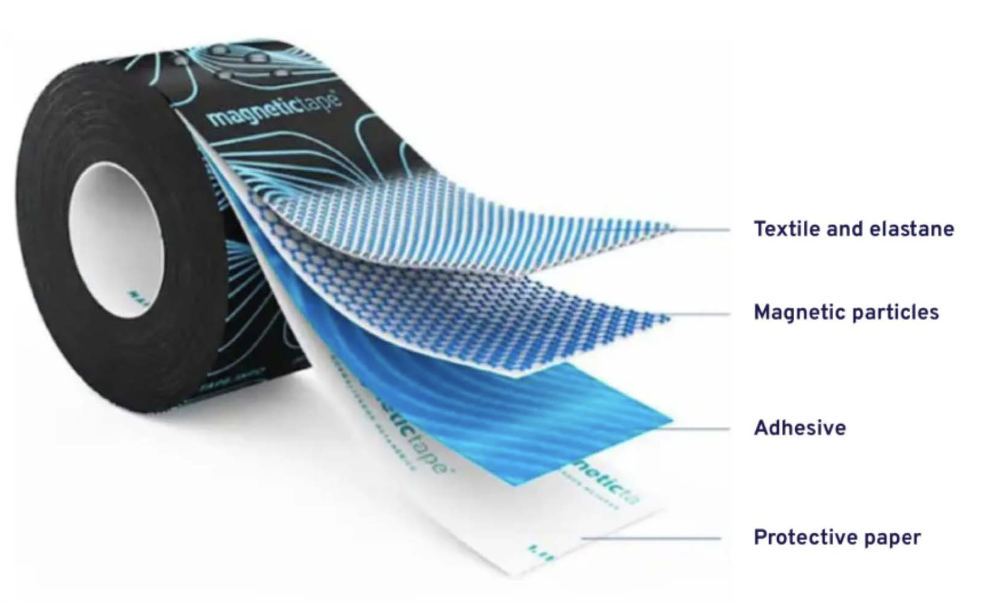
Magnetic Tape®, developed by Selva-Sarzo, resembles standard kinesiology tape but contains embedded magnetic particles that generate low-intensity magnetic fields upon skin contact. These fields do not require external power sources, which makes the tape easy to apply and maintain in clinical and community settings.
The hypothesis underpinning Magnetic Tape® is that electromagnetic fields at low intensities can modulate neural activity by influencing the membrane potentials of keratinocytes and nearby nerve fibers. When these cells are stimulated, they release biochemical signals that can travel along nerve pathways and influence distant functions, such as vascular tone, muscle activation, or pain perception.
Research led by Dr. Sillevis explored this concept in a variety of clinical conditions and confirmed that Magnetic Tape® not only adheres to the theoretical principles of neuromodulation but also produces measurable results in human subjects.
3. Clinical research on low back pain
Low back pain (LBP) is among the leading causes of disability worldwide. Its persistent nature and multifactorial etiology make it a challenging condition to manage. Dr. Sillevis’s team conducted a randomized, controlled trial on patients with chronic nonspecific LBP. Participants received either Magnetic Tape® or standard kinesiology tape over paraspinal muscles. Researchers measured variables including pressure pain threshold (PPT), changes in pupil diameter, an indirect marker of sympathetic nervous activity, and patient-reported pain scores.
Findings revealed statistically significant improvements in the Magnetic Tape® group, including an altered nervous system activity and heightened pain thresholds. These results were not mirrored in the placebo group, reinforcing the notion that the tape’s magnetic properties, and not just its mechanical support or sensory effects, were responsible for the observed changes.
Patients reported enhanced comfort and functional mobility during daily activities. For clinicians, this suggests a novel adjunct for conservative management of chronic LBP, with minimal risk and potential long-lasting effects.
4. Expanding applications: Cervical spine and autonomic effects
The cervical spine plays a vital role in coordinating movement, sensory input, and autonomic nervous system (ANS) function. Disruption in this region can result in headaches, vertigo, visual disturbances, and postural instability. In one of his pioneering studies, Dr. Sillevis applied Magnetic Tape® to the cervicothoracic junction of healthy individuals and measured its effect on cervical range of motion and pupil diameter with automated pupillometry.
Results showed a bilateral increase in pupil size post-application, suggesting a stimulation of the sympathetic pathway. Additionally, participants demonstrated improved range of motion in upper cervical rotation and increased performance in deep neck flexor endurance tests. This indicated not only an autonomic response but also a potential enhancement in motor control and muscle performance.
The implication is clear: Magnetic Tape® may serve as a bridge between musculoskeletal and autonomic therapeutic strategies, with relevance for conditions ranging from cervicogenic dizziness to whiplash-associated disorders.
5. Systemic neuromodulation: Beyond local effects
One of the most exciting discoveries in Dr. Sillevis’s research has been the observation that Magnetic Tape® applications have systemic effects beyond their immediate placement site. In a crossover clinical study, participants with chronic pain experienced improved ankle range of motion and elevated pressure pain thresholds in areas distant from the tape placement. This suggests a coordinated response within the central nervous system, possibly involving segmental spinal reflexes and supraspinal modulation.
Dr. Sillevis emphasizes that these systemic effects may redefine how therapists approach regional dysfunctions. Rather than treating only the symptomatic area, clinicians can use Magnetic Tape® to stimulate related dermatomes and fascial lines, producing changes across the kinetic chain. This opens the door to integrative, whole-body rehabilitation approaches guided by a deep understanding of neuroanatomy and sensorimotor feedback loops.
6. Superficial Neuromodulation® as a clinical framework
Superficial Neuromodulation® (SNM), developed and formalized by Dr. Fransisco Selva- Sarzo, is a conceptual model that helps clinicians systematically approach patient assessment and intervention using Magnetic Tape®. At the heart of SNM is the belief that dysfunction in the nervous system, whether segmental or systemic, can be influenced through precise skin-level stimulation.
The SNM model takes into account developmental embryology, dermatome distribution, and neurovascular maps to inform where Magnetic Tape® should be applied. Clinicians are encouraged to test for change in real time, before and after application, validating the neurological impact on functional movement and pain sensitivity. In clinical education settings, Dr. Selva- Sarzo has taught hundreds of practitioners to adopt this model, enhancing their ability to make evidence- based, patient-specific decisions.
7. Patient-centered case studies
To illustrate the real-world impact of Magnetic Tape®, there are several documented case studies showing measurable clinical gains. In one case, a patient with cervicogenic headache experienced an immediate reduction in pain intensity and restoration of cervical mobility following tape application to C2-C3 dermatomes. In another case, an athlete recovering from hamstring strain regained full functional strength within days of adjunctive Magnetic Tape® treatment.
These anecdotal reports, while not substitutes for large trials, provide valuable insight into the practical and accessible nature of this technology. The cases are used in workshops and seminars led by Dr. Selva-Sarzo to train future clinicians in recognizing patterns of dysfunction and selecting appropriate neuromodulatory strategies.
8. Educational and public health impact
As a faculty member and researcher, Dr. Sillevis has extended his influence beyond the lab through lectures, peer-reviewed publications, and professional training sessions. His work on Magnetic Tape® has inspired physical therapy programs to integrate neuromodulation into curricula, promoting a deeper understanding of the interaction between skin, nerves, and healing.
From a public health perspective, Magnetic Tape® may offer an important alternative to pharmacologic interventions, particularly amid the opioid crisis. Its non-invasive, side-effect-free application makes it suitable for populations who are elderly, pediatric, or sensitive to medication. By promoting affordable, accessible pain management tools, Dr. Sillevis contributes to broader efforts to reduce healthcare disparities and empower communities through self-care education.
9. Future research and global collaboration
Looking ahead, Dr. Sillevis is expanding research partnerships internationally to explore how Magnetic Tape® and Superficial Neuromodulation® can be adapted across healthcare systems. Projects are underway investigating the tape’s role chronic pain and neurological conditions.
Emerging technologies, including wearable sensors and AI-assisted diagnostics, may further enhance Magnetic Tape®’s integration into rehabilitation. As principal investigator, Dr. Sillevis is also exploring funding avenues to support long- term outcome studies and translational research that bridges the gap from clinic to community.
10. Conclusion: Dr. Sillevis’s vision for the future
The journey of Magnetic Tape® from conceptual tool to clinically validated intervention is a testament to the vision, and scientific contribution of Dr. Rob Sillevis. Through his interdisciplinary research and passionate teaching, he has redefined how therapists view the skin’s role in nervous system regulation.
By advancing a holistic, accessible, and patient- centered model of care, Dr. Sillevis continues to inspire clinicians and researchers around the world. Magnetic Tape® and the principles of Superficial Neuromodulation® are not just innovations, they are stepping stones toward a more integrated future in rehabilitation science.
11. Innovation and health policy alignment
Magnetic Tape® and the concept of Superficial Neuromodulation® align closely with public health policy goals aimed at reducing chronic pain, minimizing opioid use, and expanding access to non-invasive therapies. Dr. Rob Sillevis’s research presents Magnetic Tape® as a low-cost, scalable, and evidence-informed intervention that can be deployed across community clinics, veteran care settings, and rural health initiatives. Its minimal need for equipment or specialized infrastructure makes it an ideal candidate for inclusion in public health toolkits, particularly for underserved populations.
Moreover, Magnetic Tape® aligns with the U.S. Department of Health and Human Services (HHS) objectives under the Healthy People 2030 framework, especially those related to chronic pain management, mental health integration, and disability rehabilitation. By offering a safe alternative to pharmacologic treatments, Magnetic Tape® supports health equity and expands the treatment paradigm for musculoskeletal conditions.
12. Accessibility and cost-effectiveness in rehabilitation
Cost remains a significant barrier to accessing long-term rehabilitative care. Insurance caps, co-pays, and out-of-pocket fees often limit the continuity of therapy that patients need to recover from chronic or disabling conditions. Dr. Sillevis’s research on Magnetic Tape® demonstrates that inexpensive interventions can yield clinically meaningful outcomes, especially when applied within a structured, evidence-based model such as Superficial Neuromodulation®.
A single roll of Magnetic Tape® can provide multiple treatment sessions, and once applied, the therapeutic effect persists without the need for technician supervision or active participation. This presents a novel opportunity for cost-saving in both acute and chronic care models. Government agencies and healthcare payers could consider pilot programs to integrate Magnetic Tape® into rehabilitative care bundles, particularly in post- acute or home-health settings.
13. Workforce training and educational expansion
The successful integration of any therapeutic innovation into the healthcare system requires workforce training and curriculum development. Dr. Sillevis has already incorporated Superficial Neuromodulation® into academic and continuing education courses training clinicians across disciplines.
Public institutions and state-funded universities can play a critical role in expanding access to this training. Embedding neuromodulation principles into rehabilitation science programs will ensure that future providers are equipped to offer low-cost, high-impact therapies that align with modern neurophysiological principles. Such an initiative would also support workforce diversification, as Magnetic Tape® application does not require high levels of capital investment or specialist credentialing.
14. Community implementation and case use scenarios
Magnetic Tape® is uniquely suited for community- based care delivery. It can be used in mobile health units, school-based physical therapy services, senior living facilities, and even correctional institutions, anywhere access to standard rehabilitative care may be limited. In one case documented a homebound elderly patient with post-stroke shoulder pain was able to regain functional movement through repeated application of Magnetic Tape® by a visiting therapist. The patient, who had limited tolerance for conventional electrical stimulation therapies, tolerated the tape well and demonstrated sustained gains in range of motion and daily activity participation.
Such cases suggest a public health infrastructure could benefit from integrating Magnetic Tape® into federally qualified health centers (FQHCs) or the Veterans Health Administration. Pilot studies in these settings would allow for broader evaluation of outcomes, compliance, and feasibility under typical community care conditions.
15. Open science and interdisciplinary collaboration
The success of Magnetic Tape® research is not just due to its scientific rigor, but also to the collaborative and transparent model Dr. Sillevis has employed. His work has brought together researchers all working toward a shared goal of non-invasive pain and mobility solutions.
This approach aligns with the principles of open science and interdisciplinary innovation promoted by and similar platforms. Continued funding for collaborative pilot studies, open-access publishing, and government-academic partnerships will be key to advancing Magnetic Tape® as a national model of affordable, non-drug rehabilitation. Furthermore, the insights gained from Magnetic Tape® research can help shape policy guidelines on therapeutic product evaluation, reimbursement strategies, and training standards in emerging health fields.
16. Call to action for policymakers
Policymakers are in a unique position to support the transition of Magnetic Tape® from research innovation to standard care practice. By endorsing pilot programs, funding comparative effectiveness research, and incentivizing education in non- invasive modalities, state and federal agencies can accelerate adoption of cost-effective alternatives to chronic pain treatment.
Dr. Sillevis’s work serves as a model for how translational research can address both clinical and societal needs. Incorporating Magnetic Tape® into national rehabilitation frameworks, particularly for populations with limited access to traditional care, represents a forward-thinking approach that aligns with transparent and inclusive health policy values—transparency, community engagement, and evidence-driven decision-making.