Peripapillary intrachoroidal cavitation and myopic peripapillary changes: Optical Coherence Tomography analysis
Myopia, …More than just a refractive error
Myopia is a major contributor to severe visual impairment.1 By 2050, 50% of the world’s population will be myopic,2 leading to an increase in myopia-related complications.3 Myopia constitutes a public heath problem.
Beyond what is well-known, myopia is characterized by an anteroposterior elongation of the eyeball, leading to numerous detrimental structural changes and visual impairment.4
Recently, advances in optical coherence tomography (OCT) have highlighted the structural changes associated with myopia.5-8 However, there is a need to refine the link between these changes and the associated visual impairment. Here, we present the myopia-related optic nerve changes detected by OCT.
Peripapillary staphyloma… Not so insignificant
The thinning and softening of the eye wall associated with myopic elongation favor the appearance of localized external protrusions, called posterior staphylomas.
The presence of a posterior staphyloma in an eye is a hallmark of pathological myopia, a term referring to a myopic eye with myopia-related visual impairment.4
When the protrusion is located around the optic nerve head (also called the optic disc), it is called peripapillary staphyloma (PPS).9 The OCT characteristics of a PPS are well-defined7 and are presented in Figure 1. In addition to PPS, other myopic changes affect the optic disc.
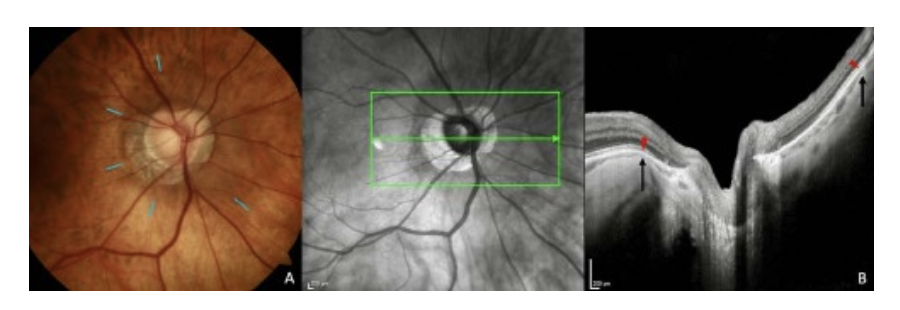
(A) Fundus image. The PPS shows slight pigmentary changes at its edges (blue lines). (B) The optical coherence tomography section is along the arrow in the infrared image. The sclera between the black arrows, including the optic nerve is bowed posteriorly with a steeper local curvature than adjacent scleral regions. The choroid shows thinning (between red arrowhead and black arrow) at the edges of PPS, followed by a rethickening towards the optic nerve. Abbreviation: PPS = peripapillary staphyloma.
Source. Ehongo A. Doctoral thesis in Medical science (2024). Free University of Brussels. Optical coherence tomography analysis of peripapillary intrachoroidal cavitation. Clinical implications for highly myopic eyes, page 20.
Disc Ovalization… Resulting from disc changes in all three spatial axes
Usually, the optic disc is slightly vertically oval or round (Figure 2.A), with individual variations. Myopic discs have more oval shapes (Figure 2.B). The process of optic disc ovalization during myopic elongation of the eye is well documented by OCT.10 Disc ovality is quantified by using the ratio of the shortest disc diameter to the longest disc diameter; this is called the disc ovality index, as we will see later. A component of the oval configuration of the optic disc is explained by viewing the optic disc in one plane, while myopic changes involve rotation of the optic disc around any of the three geometric axes.
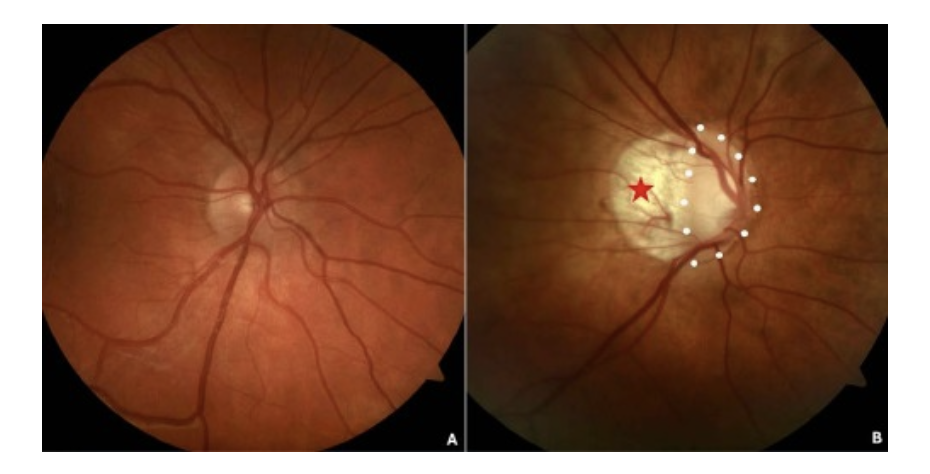
(A) A slightly oval non-myopic disc. (B) A myopic optic disc with a pronounced oval configuration (dotted white line) and a temporal conus (red star). (myopic conus = crescent).
Source. Ehongo A. Doctoral thesis in Medical science (2024). Free University of Brussels. Optical Coherence Tomography analysis of Peripapillary intrachoroidal cavitation. Clinical implications for highly myopic eyes, page 23.
Myopic conus … It reflects the disappearance of all layers of the eyewall, except for the sclera
The myopic conus (also called conus temporalis or myopic crescent) is a crescent-shaped atrophic area partly bordering the disc (Figure 3.A). It is acquired during the myopic elongation of the eye.10
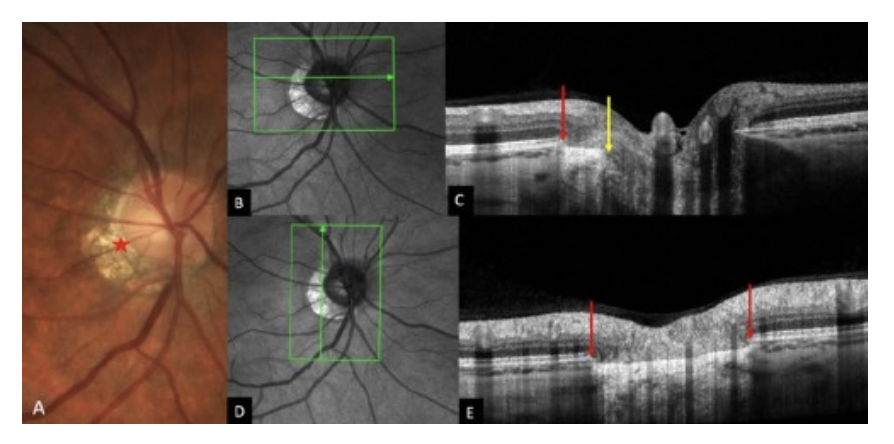
(A) Fundus image of an eye exhibiting a γPPA (red star). (B) Infra-red image with the green arrow indicating the location of section (C). (C) There is a disparity between the end of Bruch’s membrane (red arow) and the scleral opening (yellow arrow). γPPA is between the yellow and red arrows. (D) Infra-red image with the green arrow indicating the location of section (E). (E) γPPA is between the ends of BM (red arrows). Abbreviation: Gamma Peripapillary atrophy = γPPA.
Source. Ehongo A. Doctoral thesis in Medical science (2024). Free University of Brussels. Optical coherence tomography analysis of peripapillary intrachoroidal Optical Coherence Tomography analysis of Peripapillary intrachoroidal cavitation. Clinical implications for highly myopic eyes, page 67.
It reflects a disparity between the termination of Bruch’s membrane and the opening of the scleral canal (Figure 3.B-C). Within the conus, histology reveals the disappearance of all structures of the ocular wall, except the sclera,11 a feature well highlighted on OCT sections (Figure 3.D-E). It is also referred to as gamma peripapillary atrophy (γPPA) based on histological and OCT findings (other types of atrophy, namely alpha and beta, are not discussed in this work). OCT reveals a relative posterior positioning of the optic disc side with γPPA (Figure 4).
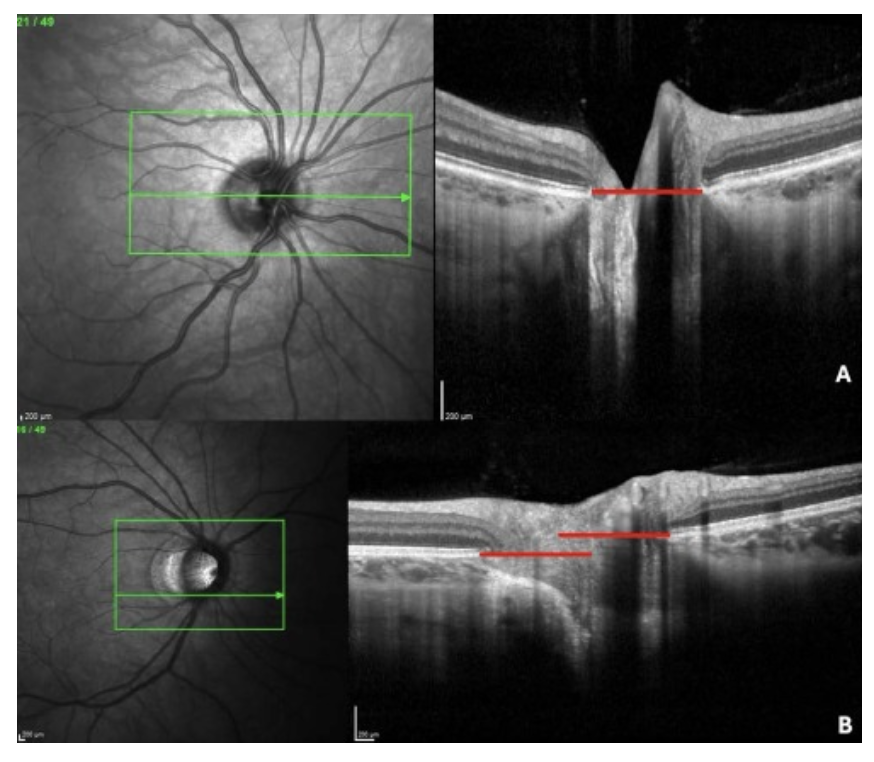
Figure 4. Myopic optic disc. Posterior positioning of the side with Gamma Peripapillary atrophy (γPPA).
Sections are along the green arrow in the infrared image. (A). Slightly oval non-myopic optic disc. Both sides are in the same plane (highlighted by the red line). (B) Myopic optic disc with a pronounced oval configuration. The relative posterior positioning of the side of the optic disc with γPPA compared to the opposite side is highlighted by the space between the red lines.
Source: Ehongo A. Doctoral thesis in medical sciences (2024). Free University of Brussels. Optical coherence tomography analysis of peripapillary intrachoroidal cavitation. Clinical implications for highly myopic eyes. Presentation to the public defense.
Peripapillary intrachoroidal cavitation (PICC)… In reality, it is a suprachoroidal detachment
PICC is a well-circumscribed yellow-orange lobular lesion located at the outer border of the myopic conus12 (Figure 5.A). Advances in OCT have clarified that PICC is a suprachoroidal detachment,5-8 (Figure 5.B-C). The multifaceted appearance of PICC is well known and results from the location and orientation of the slices.5, 6, 8 On OCT sections crossing the optic disc, it appears as a triangular thickening with its base against the optic nerve (Figure 5.B-C).
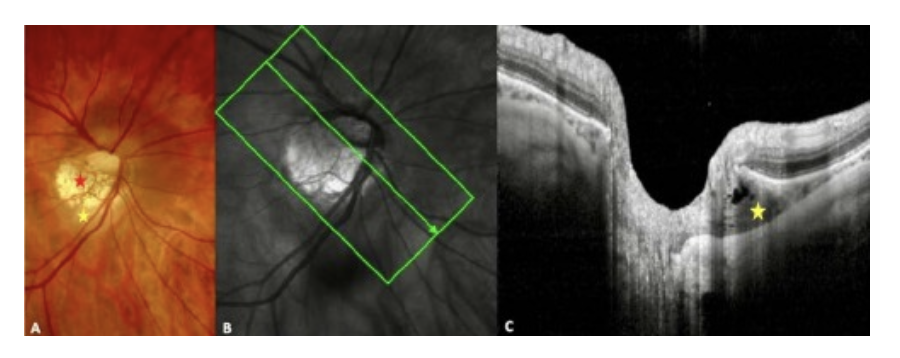
(A) Fundus image. Myopic conus = red star. (B) Infrared image with the green arrow showing the location of the slide (C). (C) The Peripapillary intrachoroidal cavitation is the intrachoroidal hyporeflective triangular thickening with the base against the optic nerve. It is highlighted by the yellow star in A and C.
Source. Ehongo A. Doctoral thesis in Medical science (2024). Free University of Brussels. Optical coherence tomography analysis of peripapillary intrachoroidal Optical Coherence Tomography analysis of Peripapillary intrachoroidal cavitation. Clinical implications for highly myopic eyes, page 67.
The typical myopic disc… In fact, it is a combination of several of these changes
Generally, in each myopic disc, several of these entities coexist, each with a varying degree of severity. The consistent location of the PICC at the outer border of the conus is established. Furthermore, we have documented that the prevalence of PICC in eyes with γPPA is 10.4%, while 20.5% of eyes with PPS have PICC.8, 13 More interestingly, we found that all eyes with PICC combine both PPS and γPPA8, 13 (Figure 5.B-C).
Relevance of understanding myopic peripapillary changes… Avoiding diagnostic errors
Interest in myopic peripapillary changes stems from their functional implications, primarily visual field deficits.6,14 Especially since these deficits resemble those observed in glaucoma, leading to diagnostic uncertainty.15 Therefore, efforts are being made to improve the ability to distinguish myopic deficits from those of glaucoma, mainly normal- tension glaucoma. Indeed, although myopic changes tend to be less progressive, glaucoma, the leading cause of irreversible blindness,16 requires early diagnosis to enable appropriate management. Finally, a quantitative correlation between structural myopic changes and the severity of associated visual defects would be valuable.
Eye movements: What is the link with peripapillary myopic complications
Although the pathogenesis of peripapillary myopic complications remains to be elucidated, recent biomechanical studies have shed new light on their occurrence. It has been suggested that the peripapillary myopic deformities are promoted by the pulling force of the optic nerve sheaths on their scleral insertions. 5-8, 17, 18
Moreover, the amplitude of the forces deployed by these sheaths reaches that of the extraocular muscles.19 Thus, this concept of deformation of the eyeball by traction or compression exerted by structures inserted on its surface deserves to be studied. It highlights the impact of extraocular muscles on the eyeball during their action, which constitutes a potential advance in the understanding of the pathogenesis of posterior staphyloma, thus justifying further investigations.
Quantification… to standardize myopic changes, the basis of large-scale studies
The aforementioned disc ovality index is an approach for quantifying the degree of disc deformation. An ovality index ≤ 0.8 is considered low. Studies analyzing myopic peripapillary changes have demonstrated their clinical relevance.
- Low disc ovality index and PICC. In highly myopic eyes, an intra-individual inter-eye comparison showed that the prevalence of PICC was higher in the eyes with a low ovality index.20 Additionally, we documented that the only discriminating factor between eyes combining PPS and γPPA whether PICC was present or absent, was a lower ovality index in the group with PICC.8,14
- Low disc ovality index and visual field defects. In highly myopic eyes, the prevalence of visual field defects was shown to be significantly higher in eyes with a low ovality index.21 Furthermore, we found that in eyes with PICC, the prevalence of visual field defects was higher in eyes with a low ovality index.8,14
- Finally in myopic eyes combining PPS and γPPA, we found that the prevalence of visual field defects was higher in the presence than in the absence of PICC. 8,14
A quantitative approach to standardize the characteristics and severity of myopic complications for large-scale studies is warranted.
In conclusion, Myopia is recognized as a public heath problem. Future directions include defining and quantifying the severity of myopic changes in an eye, as well as the significance of the impact of eye movements on an eye. Efforts are being made to understand the mechanisms promoting myopia and leading to its complications in order to reverse its increasing prevalence and associated burden.


