Researchers at King’s College London have developed a novel daily pill, KCL‑HO‑1i, that turns off tumour‑guarding macrophages and boosts chemotherapy effectiveness
A team of scientists at King’s College London has unveiled a promising new drug, dubbed KCL‑HO‑1i, designed to enhance the effectiveness of chemotherapy in cancers that have developed resistance. The breakthrough comes after uncovering how macrophages in the tumour microenvironment produce the enzyme heme oxygenase-1 (HO-1) to shield tumours from immune attack.
Lab success in chemotherapy-resistant tumours
The first lab study of the drug, named KCL-HO-1i, has shown that it boosts the effectiveness of chemotherapy in mouse models, making chemotherapy-resistant tumours vulnerable.
“We discovered that macrophages guard the tumour and can block the effects of chemotherapy,” said Professor James Arnold, head of the Tumour Immunology Group at KCL and one of the co-leads of the research. “They’re acting as gatekeepers, stopping cancer-fighting immune cells from coming in and supporting the treatment, but by targeting the right pathway, we can open the door.”
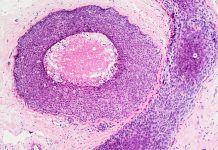
The researchers first set up a lab to study the role of macrophages in and around tumours in the early 2010s. The team soon realised that these “tumour-associated” macrophages produce a high amount of an enzyme called heme oxygenase-1 (HO-1), which has been the focus ever since.
“It’s an enzyme that’s almost become part of the family,” Arnold said. “I’ve spent many sleepless nights trying to understand how it works.”
The team discovered that HO-1 can shield tumours from the body’s defences.
“What we ended up finding was that these macrophages, and heme oxygenase-1, are sitting around blood vessels in the tumour and playing quite fundamental roles in regulating the immune response against cancer, which has major implications for the efficacy of chemotherapy,” explained Arnold.
Developing a daily pill for patients
Typically, chemotherapy kills fast-dividing cells, independently of the immune response, which targets abnormal cells. However, as the research progressed, the team discovered additional evidence that the most effective chemotherapies appear to harness the immune response against cancer, activating cancer-killing cells known as T cells.
“The macrophages think they’re meant to protect the cancer, so they make heme oxygenase-1 to keep T cells out,” says Arnold. “When we targeted the heme oxygenase-1 using KCl-HO-1i, we found that chemotherapy was much more effective – purely because it could generate a stronger immune response in the cancer.”
The researchers called upon KCL colleagues James Spicer, Professor of Experimental Cancer Medicine, and Miraz Rahman, Professor of Medicinal Chemistry, who have completed extensive research into a heme oxygenase-1 blocker as a treatment for jaundice in newborns. Using this expertise, Arnold and his team developed KCL-HO-1i, a new drug that can be given as a daily pill. That means people receiving chemotherapy could take it at home between treatment sessions. It has the potential to make hospital treatments more effective without requiring additional time in the hospital.
“This is all thanks to so much teamwork across different disciplines,” said Arnold. “We realised this could be a new drug opportunity for people with cancer, and that motivated so many talented individuals, like Dr Meriem Bahri, the lead author of our paper, to get us to this point. The paper really brings all this work together, so this is a lovely position to be in.”