Scientists have directly visualised alpha-synuclein oligomers in human brain tissue, a key trigger in Parkinson’s disease, offering new avenues for early diagnosis and treatment
For the first time, researchers from the University of Cambridge, UCL, the Francis Crick Institute, and Polytechnique Montréal have directly observed and quantified alpha-synuclein oligomers in human brain tissue. These protein clusters, long suspected to trigger Parkinson’s disease, had previously eluded detection. The breakthrough, published in Nature Biomedical Engineering, could revolutionise early diagnosis and pave the way for targeted therapies.
New research visualises elusive oligomers that precede lewy bodies
Parkinson’s disease affects around 166,000 people in the UK, and this number continues to rise. By 2050, the number of people with Parkinson’s is expected to double to 25 million. There are no drugs available to slow or stop the disease itself.
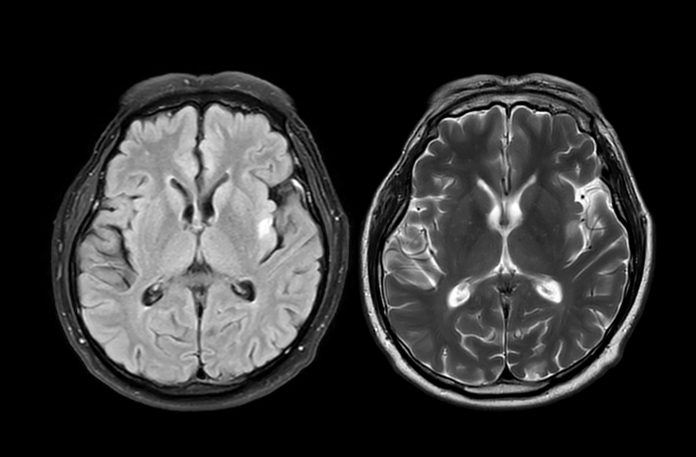
For more than a century, doctors have recognised Parkinson’s by the presence of large protein deposits called Lewy bodies. But scientists have suspected that minor, earlier-forming oligomers may cause damage to brain cells. Until now, these oligomers were too small to see – just a few nanometres long.
“Lewy bodies are the hallmark of Parkinson’s, but they essentially tell you where the disease has been, not where it is right now,” said Professor Steven Lee from Cambridge’s Yusuf Hamied Department of Chemistry, who co-led the research. “If we can observe Parkinson’s at its earliest stages, that would tell us a whole lot more about how the disease develops in the brain and how we might be able to treat it.”
Ultra-sensitive imaging uncovers the earliest markers of Parkinson’s disease
A new technique, developed by the researchers, is called ASA-PD (Advanced Sensing of Aggregates for Parkinson’s Disease), and uses ultra-sensitive fluorescence microscopy to detect and analyse millions of oligomers in post-mortem brain tissue.
Since oligomers are so small, their signal is very weak. ASA-PD works by maximising the signal whilst decreasing the background, dramatically boosting sensitivity to the point where individual alpha-synuclein oligomers can be observed and studied.
“This is the first time we’ve been able to look at oligomers directly in human brain tissue at this scale: it’s like being able to see stars in broad daylight,” said co-first author Dr Rebecca Andrews, who conducted the work when she was a postdoctoral researcher in Lee’s lab. “It opens new doors in Parkinson’s research.”
The team analysed post-mortem brain tissue samples from people with Parkinson’s and compared them to healthy individuals of similar age. They found that oligomers exist in both healthy and diseased brains, including those with Parkinson’s. However, the main difference between disease and healthy brains was the size of the oligomers, which were larger, brighter and more numerous in disease samples, suggesting a direct link to Parkinson’s disease progression.
Furthermore, the researchers identified a subclass of oligomers that appeared only in patients with Parkinson’s disease, which could be the earliest visible markers of the disease.
“This method doesn’t just give us a snapshot,” said Professor Lucien Weiss from Polytechnique Montréal, who co-led the research. “It offers a whole atlas of protein changes across the brain, and similar technologies could be applied to other neurodegenerative diseases like Alzheimer’s and Huntington’s.
“Oligomers have been the needle in the haystack, but now that we know where those needles are, it could help us target specific cell types in certain regions of the brain.“
“The only real way to understand what is happening in human disease is to study the human brain directly, but because of the brain’s sheer complexity, this is very challenging,“ said Professor Sonia Gandhi from The Francis Crick Institute, who co-led the research. “We hope that breaking through this technological barrier will allow us to understand why, where and how protein clusters form and how this changes the brain environment and leads to disease.”