NICE advises adding quick spine checks to routine bone scans to detect hidden vertebral fractures earlier and prevent pain and disability
The National Institute for Health and Care Excellence (NICE) has recommended that quick spine checks, known as vertebral fracture assessments, be added to routine bone density scans to help identify hidden spine fractures earlier and reduce long-term pain and disability in individuals with osteoporosis. This move addresses a significant gap, as around 70% of spinal fractures linked to osteoporosis currently go undiagnosed, meaning many people miss out on bone-strengthening treatment that could protect their quality of life.
Osteoporosis affects millions as NHS expands early detection with new scanner
Osteoporosis affects around 3.5 million people in the UK, with around 2.95 million in England alone. Fractures of the vertebra are one of the most common types of osteoporosis-related fractures and signal the increased likelihood of further bone problems later. Approximately 549,000 new fragility fractures occur annually in the UK, including 105,000 hip fractures, 86,000 vertebral fractures, and 358,000 other fractures.
To further support the early identification and treatment of osteoporosis-related fractures, the NHS has rolled out 13 new DXA bone scanners across hospitals in England, delivering an additional 29,000 scans per year.
NICE proposes routine spine checks to detect fractures earlier
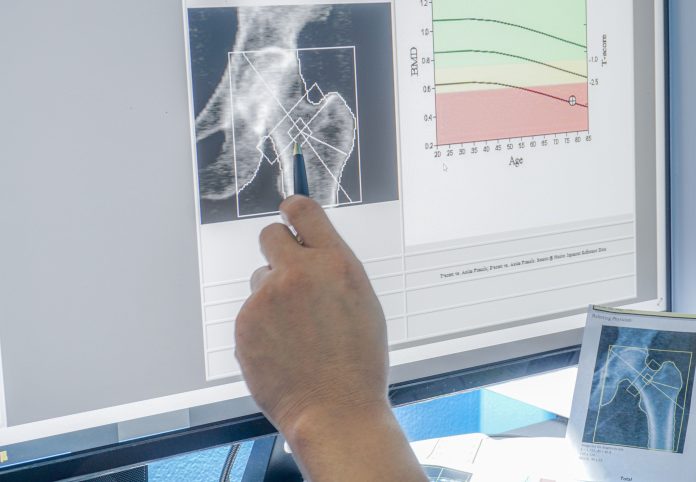
In the draft osteoporosis guideline, launched for consultation, NICE has recommended that healthcare practitioners consider offering vertebral fracture assessment (VFA) during dual-energy X-ray absorptiometry (DXA) bone mineral density scans in people aged 50 and over. Adding vertebral fracture assessment (VFA) to routine bone scans could allow preventive measures to be taken to avoid significant pain and disability from bone fractures later in life. Spotting hidden fractures early means doctors can offer bone-strengthening treatment to prevent further breaks and maintain quality of life.
People considered at risk of fragility fractures are usually assessed using a risk prediction tool (either FRAX or QFracture), and if their risk score is 10% or more, they are offered a DXA scan. However, the draft guidance recommends that DXA scans be automatically offered to people who have had either a previous hip or vertebral fragility fracture or 2 or more fragility fractures, as they are likely to have a risk score above 10%.
“Vertebral fractures can have a devastating impact on people’s quality of life. Introducing vertebral fracture assessments during routine bone density scans will help healthcare professionals get the right care to people sooner,” added Eric Power, interim director of the Centre for Guidelines.
Eric added, “Osteoporosis affects millions in England. This guidance helps professionals target care to those at highest risk, improving quality of life and using NHS resources efficiently.”