Doctors have delivered gene therapy during heart bypass surgery for the first time, aiming to strengthen blood vessels and prevent future heart failure
Doctors in Scotland have treated the world’s first patient with a new cardiac gene therapy during routine heart bypass surgery, marking a major breakthrough in heart disease treatment. The experimental therapy alters genes in graft blood vessels to make them stronger and longer-lasting, potentially reducing the risk of future heart failure and repeat surgeries. If successful, the trial could significantly influence treatment approaches for heart disease patients globally, not just in Scotland, by potentially setting a new standard of care.
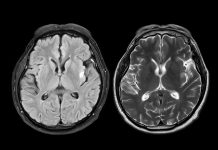
How heart bypass surgery works
Heart bypass surgery improves the blood flow to the heart and is a life-saving treatment for patients with coronary heart disease. The process uses one artery and two or more veins as bypass grafts; these healthy blood vessels bypass a narrowed or blocked artery, creating a new route for blood flow.
Vein grafts can fail because they’re not designed to withstand the heart’s high blood pressure.
A breakthrough gene therapy trial
The PROTECT study, led by NHS Greater Glasgow and Clyde and the University of Glasgow in Collaboration with NHS Golden Jubilee and the University of Edinburgh, is trialling a new gene therapy designed to support newly grafted blood vessels.
This treatment works by introducing a gene encoding the TIMP-3 protein into the vein to be grafted.
TIMP-3 is involved in tissue remodelling. Higher levels of the protein could help prevent blood vessel thickening and blockages over time.
The researchers have developed a method of treating the graft directly at the time of surgery, safely and efficiently delivering the gene therapy to the affected tissue before grafting into the heart.
The team hope the treatment will extend a patient’s healthy life expectancy and reduce the need for further surgeries.
“Our team has developed a new approach to prevent vein graft failure. The new gene therapy has been developed over more than two decades of teamwork involving many experts.
We are delighted to be leading this new study, which is designed to clarify the feasibility and potential benefits of this new therapy for patients undergoing heart bypass surgery,” commented Professor Colin Berry, University of Glasgow, NHS Glasgow and Greater Clyde, and NHS Golden Jubilee.
“I’m hugely grateful to the Medical Research Council and British Heart Foundation for helping the team translate this laboratory discovery to clinical evaluation. We have faced many challenges, but our interdisciplinary team and funders working together have enabled the trial to become a reality,” commented Professor Andrew Baker, Academic Lead for the study, University of Edinburgh and Visiting Professor at the University of Glasgow.
“This pioneering study is an inspiring reminder of how far gene therapy, which was once a distant scientific ambition, has come. Research funding from the BHF to Professor Andrew Baker over many years laid the groundwork for this study, generating the knowledge, experience, and proof-of-concept data needed to move this research out of the lab and into the clinic. In partnership with the MRC, continued BHF funding has enabled Professors Berry and Baker to begin the clinical trials necessary to prove the value of this new therapy. We look forward to seeing the results of this exciting trial in a few years,” added Professor James Leiper, Director of Research, British Heart Foundation.