A new immunotherapy for a severe form of blood cancer will soon be available on the NHS, offering new hope to adults whose disease has returned or stopped responding to conventional treatment
The personalised CAR T-cell therapy, known as obe-cel, has shown incredible results in clinical trials and is expected to begin reaching eligible patients within weeks through specialist centres across England.
A personalised approach to cancer treatment
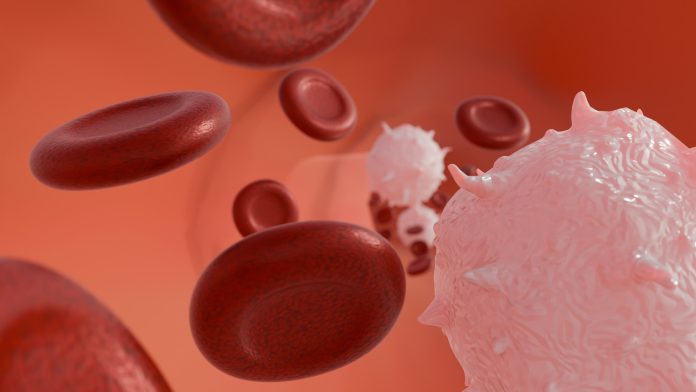
Obe-cel is a form of CAR T-cell therapy, also known as “living medicine.” The treatment involves collecting a patient’s own immune cells and re-engineering them in a laboratory so they can recognise and attack cancer cells more effectively. Once modified, these cells are infused back into the patient’s bloodstream, where they find and destroy leukaemia cells.
For people with B-cell acute lymphoblastic leukaemia (B-cell ALL), the arrival of obe-cel represents a significant shift in treatment options. The therapy will be available to adults aged 26 and over whose cancer has relapsed or proven resistant to earlier treatments. Around 50 patients in England are expected to receive it each year following approval by the National Institute for Health and Care Excellence (NICE).
Clinical trial results
Clinical trial findings show that Obe-cel can produce profound and lasting remissions in a majority of patients. In studies, 77% of participants entered remission, and around half of those remained free of detectable cancer for more than 3 years. On average, the therapy delivered 15.6 additional months of life compared to existing treatments, a clear improvement for a disease with historically poor outcomes.
The therapy shows lower toxicity and a reduced risk of severe side effects when compared with other CAR T-cell treatments. The most common adverse reaction was Cytokine Release Syndrome, a known immune response that typically presented in mild to moderate form.
Expanding NHS access to CAR T-Cell therapies
The approval of obe-cel adds to the growing range of personalised cancer therapies accessible through the NHS since it became the first health service in Europe to offer CAR T-cell treatment in 2018. Thanks to interim support from the Cancer Drugs Fund, roll-out of the new therapy will be faster than the usual 90-day implementation period, ensuring that eligible patients begin receiving treatment as quickly as possible.
Delivery will initially take place at selected CAR T-cell specialist centres, with the number of hospitals offering the therapy expected to increase through 2026 and 2027. The design of OBE-Cel also means it could be administered in outpatient settings in the future, making it more accessible for older adults or those with additional health needs.
A home-grown innovation
Obe-cel is a clear example of success for the UK’s life sciences sector. Developed, researched, and manufactured domestically, the therapy originated from work at University College London before being brought to market by Autolus Therapeutics, a UCL spin-out company. Production will take place in Stevenage, a growing hub for cell and gene therapy manufacturing.
With approximately 800 people diagnosed with acute lymphoblastic leukaemia each year in the UK, half of them adults, the introduction of obe-cel marks a significant step forward for patient care. Current standard treatment options, such as chemotherapy, offer limited long-term survival for those with relapsed or refractory disease, with an average life expectancy after treatment of around ten months.