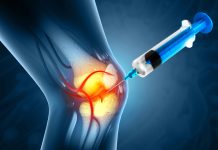
Cambridge scientists develop artificial cartilage that delivers anti-inflammatory drugs directly to inflamed joints, promising more effective, targeted arthritis relief
A team at the University of Cambridge has engineered artificial cartilage that responds to joint inflammation, releasing anti-inflammatory drugs precisely where needed. This breakthrough offers a promising new approach to treating arthritis, enhancing effectiveness, minimising side effects, and providing patients with better long-term relief.
Their results are reported in the Journal of the American Chemical Society.
Artificial cartilage to treat arthritis
During an arthritis flare-up, a joint becomes inflamed and slightly more acidic than the surrounding tissue. The new material has been designed to respond to the natural change in pH. As the acidity increases, the material becomes softer and more jelly-like, triggering the release of drug molecules that can be encapsulated within its structure.
The material is designed to respond only within a narrow pH range, and the researchers assure that drugs could be released precisely where and when they are needed, potentially reducing side effects.
If the material is used as an artificial cartilage in arthritic joints, it could enable continuous treatment of arthritis, relieving pain and combating inflammation. Arthritis costs the NHS £10.2 billion annually; therefore, finding new treatment solutions is critical. This new approach could potentially significantly reduce the cost burden.
“For a while now, we’ve been interested in using these materials in joints, since their properties can mimic those of cartilage,” said Professor Oren Scherman, who is Professor of Supramolecular and Polymer Chemistry and Director of the Melville Laboratory for Polymer Synthesis. “But to combine that with highly targeted drug delivery is a really exciting prospect.”
“These materials can ‘sense’ when something is wrong in the body and respond by delivering treatment right where it’s needed,” said first author Dr Stephen O’Neill. “This could reduce the need for repeated doses of drugs, while improving patient quality of life.”
A drug delivery system triggered by chemistry
This new material is unique; the body’s own chemistry powers it. The researchers say this could pave the way for longer-lasting, targeted arthritis treatments that automatically respond to flare-ups, boosting effectiveness while reducing harmful side effects.
In laboratory tests, researchers loaded the material with a fluorescent dye to mimic how a real drug might behave. They found that at acidity levels typical of an arthritic joint, the material released substantially more drug cargo compared with normal, healthy pH levels.
“By tuning the chemistry of these gels, we can make them highly sensitive to the subtle shifts in acidity that occur in inflamed tissue,” said co-author Dr Jade McCune. “That means drugs are released when and where they are needed most.”
This approach is not limited to arthritis. It can be tailored to many medical conditions by simply fine-tuning the material’s chemistry, offering a versatile solution for a range of health issues.
“It’s a highly flexible approach, so we could in theory incorporate both fast-acting and slow-acting drugs, and have a single treatment that lasts for days, weeks or even months,” said O’Neill.
The team is focusing on testing the materials in living systems to evaluate their performance and safety in a physiological environment. If successful, their approach could pave the way for a new generation of responsive biomaterials that can treat chronic diseases with greater precision.