Without prompt treatment, a pneumothorax may progress to cardiac arrest and death. Pneumothorax develops as air becomes trapped in the pleural space from traumatic, iatrogenic, or other causes.[1] A large pneumothorax can cause hemodynamic instability, therefore early recognition is central to management.
Bedside thoracic ultrasound is rapid, portable, and may be performed with the patient upright or supine. Bedside ultrasound is more accurate than supine chest x-ray for detecting pneumothorax, with diagnostic ability approaching that of CT.[2-7]
Air is a poor medium for ultrasound waves due to its low density and slow propagation velocity. Healthy lungs contain air, and are surrounded by the highly reflective bones of the ribs. Rather than visualizing lungs directly, pulmonary ultrasound identifies various artifacts or detection of movement.
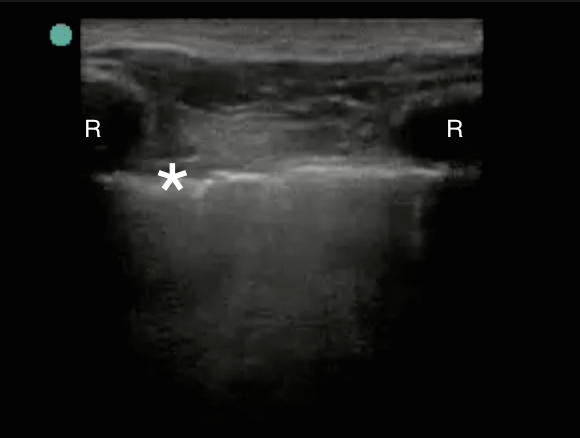
In a longitudinal view, the acoustic shadowing of the ribs marks the space where the pleural line may be identified. In Figure 1, the acoustic shadow of the ribs (R) is created by the strongly reflective bony cortex, and marks the pleural line (asterix). Since bone reflects ultrasound waves, no signal is detected behind the bony cortex, creating shadowing.
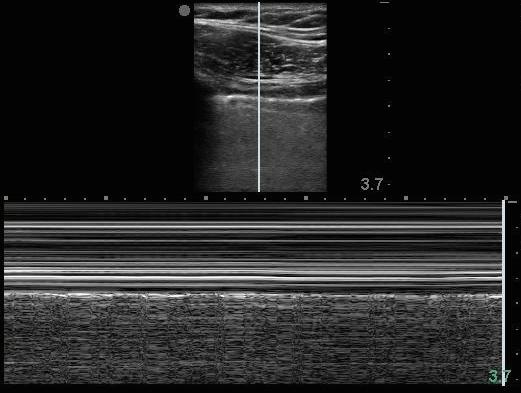
Normal pleural movement demonstrates a “shimmer sign” with B mode imaging. Poor respiratory effort, operator experience or fatigue, and other factors may complicate the identification of a “shimmer sign”. M mode imaging uses a high frequency probe to depict lung movement. Using M mode, normal lung that is moving has a homogenous granular appearance under the brightly visualized pleura. Figure 2 depicts this “seashore sign”, with the normal lung reminiscent of sand and approaching waves. The loss of granular appearing “sand” on the bottom half of the screen is indicative of pneumothorax.
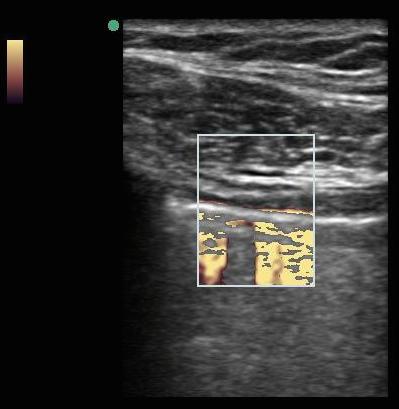
Lung sliding is also detected by Doppler. Power Doppler (Figure 3) utilizes an orange scale to detect movement relative to the transducer surface, which is more sensitive for movement as compared to the red blue Color Doppler. A patient with a pneumothorax will not have lung sliding relative to the transducer surface, and no color will be detected in the sample selected (Figure 4).

B lines, also known as comet tail artifacts, represent the common border between the interlobular septa and the alveolar wall.[1] B line artifacts start from the pleural line, and are hyperechoic, or brighter than the surrounding field. B lines move with lung sliding during respiration. In normal lung the B lines appear to wipe side to side over the stationary appearing A lines, which are the reverberation artifacts of the pleural line. The lack of B line movement also indicates pneumothorax.
As a general rule of thumb, it is recommended to visualize more than one lung field, and scan areas where there is clinical suspicion for pathology. The BRIPPED protocol is a screening tool for undifferentiated shortness of breath that may be performed with the patient in any position, and utilizes high and lower frequency probes using a portable bedside ultrasound machine. The BRIPPED protocol evaluates pneumothorax among other etiologies of shortness of breath.
Virginia Stewart
Director of Emergency Ultrasound
Director of Ultrasound Fellowship
Department of Emergency Medicine
Riverside Medical Group
Newport News, VA
Tel: 001 757 510 8197
References:
1) O’Connor AR, Morgan WE. Radiological review of pneumothorax. BMJ 2005; 330:1493
2) Kirkpatrick, A.W., et al., Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST). J Trauma, 2004; 57(2): 288-95.
3) Jalli R, Sefidbakht S, Jafari SH. Value of ultrasound in diagnosis of pneumothorax: a prospective study. Emerg Radiol 2013; 20:131
4) Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med 2010; 17:11.
5) Raja AS, Jacobus CH. How accurate is ultrasonography for excluding pneumothorax? Ann Emerg Med 2013; 61:207.
6) Alrajhi K, Woo MY, Vaillancourt C. Test characteristics of ultrasonography for the detection of pneumothorax: a systematic review and meta-analysis. Chest 2012; 141:703.
7) ALrajab S, Yousset AM, Akkus NI, Caldito G. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care 2013; 17:R208.








