The PinPoint Test is an AI-driven, affordable blood test for cancer designed to optimise NHS urgent cancer referral pathways. The Test is based on an algorithm which employs machine learning to analyse 31 standard analytes, plus the patient’s age and sex
Suspected cancer patients in England are currently referred to the NHS urgent cancer referral pathway, known as the ‘2-week wait’ (2WW). It guarantees that suspected cancer patients can see a specialist in Secondary Care within 14 days of referral.
From 1 million patients per year at its inception in 2010, 2WW referrals have grown steadily at approximately 10% per annum to 2.8 million patients in 2022.
The pressure on the system is unsustainable and the situation has only been exacerbated by the impact of COVID-19, a system shock that left cancer services reeling with delays to diagnosis and treatment.
The greater the backlogs, the further we get from a system capable of meeting the Government’s ambition of 75% of all cancers being identified early by 2028.
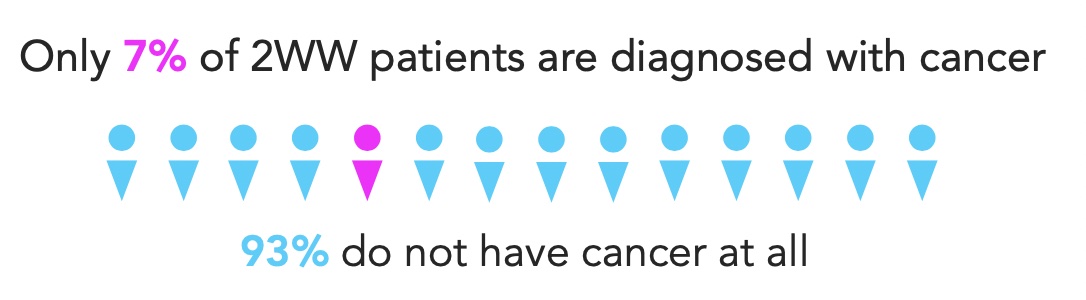
In fact, despite these soaring numbers, only 7% of patients referred are ultimately diagnosed with cancer. The remaining 93% of patients (2.6 million people in 2022) do not have cancer at all.
Even among symptomatic patients, confirming a cancer diagnosis can be like looking for a needle in a haystack, and the hunt for that needle takes time and resources; resources that could potentially be used elsewhere.
From a human perspective, every day ‘not knowing’ is a day of anxiety as patients wait for appointments, test results and diagnoses. Under the 2WW system, the latter stages of the pathway are not captured but based on the recommendations of the 2015 Cancer Strategy, a transition is already underway to shift reporting of the cancer pathway to the ‘Faster Diagnostic Standard’ (FDS). This requires that patients receive a diagnosis of cancer, or have cancer ruled out within 28 days.
Within that window of time, a system for more accurately prioritising patients by risk could be transformational for supporting early detection and preventing unnecessary testing and waits for those in the 93% at negligible risk.
At PinPoint, we don’t think the answer is bigger budgets and more machines. We see the solution as a fundamental upgrade to the approach to diagnostics for cancer patients in the NHS. We believe that providing clinicians with better tools for intelligent triage and prioritisation will enhance capacity, reduce backlogs and ensure the patients that need it most get help faster and more efficiently. So what is our solution?
Cancer diagnostics: The Pinpoint test
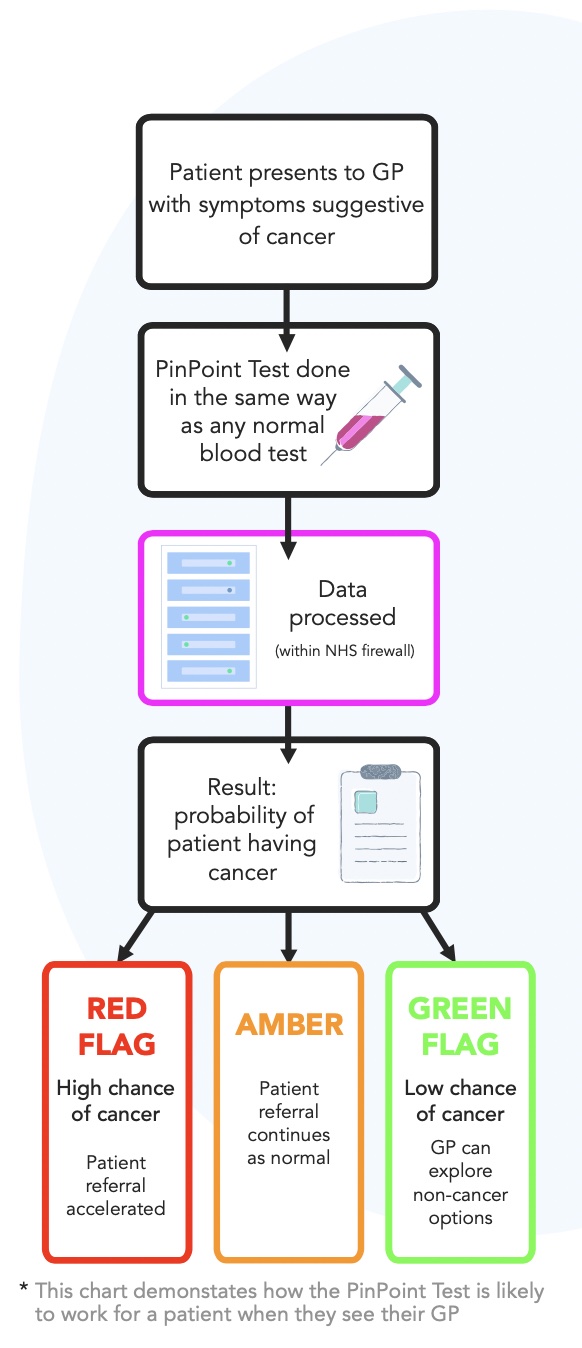
The PinPoint Test is an AI-driven, affordable blood test for cancer designed to optimise NHS urgent cancer referral pathways. The Test is based on an algorithm which employs machine learning to analyse 31 standard analytes, plus the patient’s age and sex. It can calibrate and aggregate these individual signals into one strong and highly accurate result: the chance that a patient has cancer.
The test is designed as a decision support tool to provide doctors with the information they need to more effectively triage patients when they first present with symptoms.
Those at high risk can be prioritised for rapid investigation in Secondary Care, whilst those at lowest risk can be safely ruled out of the 2WW pathway for further consultation with their GP.
The PinPoint system of red-flagging those at the highest risk for prioritisation will improve early detection, contribute to a more robust pathway and help reduce post-pandemic backlogs.
Meanwhile, our data suggest that up to 20% of current 2WW referrals could be safely ruled out via a PinPoint green flag system, equating to 560,000 patients per year (based on 2021-22 data). That’s peace of mind delivered in the time it takes to run a blood test and an opportunity for your GP to more quickly identify the appropriate onward clinical path.
Deployed at scale, we believe the PinPoint Test can deliver enhanced diagnostic capacity, shortened waiting lists and significant cost savings to the NHS.
From its very inception, the Test has been designed to address the unique challenges of the NHS and to fit seamlessly into NHS referral pathways. Clinicians have been involved from Day 1 and their input has helped shape the test as a tool to support them in the work of saving lives.
Real-world integration
The ability of any new technology to integrate quickly into the complexity of the NHS is paramount to making the right kind of impact. We understand that the best solution to the challenge of diagnostic capacity is one that can deliver improvements in patient outcomes and achieve national cancer targets, doing both at speed, without disruption or lengthy integration periods.
The PinPoint Test is designed with exactly that in mind. It does not rely on costly specialist equipment, it runs on existing NHS IT and laboratory testing systems under complete NHS control, and the test result is delivered back to clinicians through the standard systems. All data is anonymised and processed within the NHS firewall for safe-by-design data security and logistical ease of use.
To make the greatest impact where it is needed, the PinPoint Test is CE marked for the 9 most populous 2WW pathways, representing over 98% of all referrals: Breast, Gynaecological, Haematological, Head & Neck, Lower GI, Lung, Skin, Upper GI & Urological.
Software diagnostics as an app for evolving healthcare
Machine learning is the technique used to develop the PinPoint algorithm; to train it to recognise patterns across huge data sets. Over time, new data can and will be incorporated into future versions of the test for improved diagnostic performance, but despite misconceptions around the term ‘AI’, this is not an automated process. Instead, this is done by PinPoint’s superb team of data scientists and tested thoroughly before each new rollout.
Herein lies one of the greatest strengths of a product like the PinPoint Test. As the algorithm is refined and improved over time, it can be rolled out without any need for costly physical upgrades to lab equipment. Like an app on your phone, its performance will improve over time as upgrades are developed, tested and incorporated in the background. The PinPoint Test will update without the need for the NHS to invest further in infrastructure: an innovative solution for evolving healthcare.
How machine learning is unlocking the complexity of medical data to deliver the next generation of diagnostic testing
As a patient, what is the question you want answered when you receive a diagnostic test? Very simply, you want to know what (if anything) is wrong with you, so that your doctor can help you if needed or reassure you if not.
But is this the question current diagnostic tests answer? Well, sometimes.
Let’s consider blood tests. If you’re really lucky, there’s a single analyte the lab can measure that will give your doctor a clear answer. If not, there may be a combination of analytes that when looked at together, can provide an answer, but this often isn’t the case and the road to diagnosis becomes longer and less clear.
The human brain has evolved to recognise patterns and extrapolate conclusions, but there are limits to the number of interdependent data points we can process effectively at any one time. With a data set as complex and fluid as an individual patient’s biology, the absence of a red-flag test result can leave even the most experienced GP or Consultant forced to rely on intuition and a process of elimination and deduction.
But what if the answer is available in that first blood test, it’s just spread across tens or hundreds of analytes?
Cancer is a particularly challenging example. While there are a few specific cancers where a single analyte is useful (e.g., PSA for prostate cancer), for most cancers this is not the case. And yet, scientific literature reports many examples of signals that can be measured in blood and that are known to carry trace amounts of cancer information.
The difficulty is that these individual analytes are often not informative enough on their own to be useful in forming a diagnosis. An elevated platelet count might be a warning sign for cancer [1]; a range of immune-related biomarkers are associated with increased cancer risk [2]; C-reactive protein (CRP) can be elevated in ovarian cancer patients [3] and is even more significant when combined with CA-125 and HE4; serum bilirubin levels are negatively associated with both lung and cervical cancer risk [4]. The list goes on.
Some tumour markers already in use have been shown to be more broadly informative than for just the cancers they are primarily used to investigate. For example, in primary care patients with elevated CA-125 (an ovarian cancer tumour marker), not only were 10.1% of patients diagnosed with ovarian cancer but a further 12.3% were diagnosed with a completely different type of cancer [5].

Despite the name, Prostate Specific Antigen (PSA) is known to also be produced at lower levels by other tissues and to have potential as a marker for colon and breast cancer [6, 7].
All of these analytes, and others not discussed here but linked to cancer risk, are easily measured in NHS pathology laboratories. They are routine, established and importantly, they are affordable to process. Without the right tool to interpret them, however, these analytes are a largely untapped resource.
A test like PinPoint, with the ability to combine these individual signals into a single, more informative, calibrated result, has the potential to be transformative for early diagnosis. It does what a person cannot: accurately calculate a patient’s risk profile for cancer based on historic data from more patients than a GP could see in a lifetime. A simple answer to a complex question.
A surge of innovation
The PinPoint Test isn’t alone. There are several different approaches to multi-cancer early detection that are at various stages of development. Many of those more widely known are focused on the detection of circulating tumour DNA (ctDNA) in the blood. Companies in this area include GRAIL [8], CancerSEEK [9], Freenome [10] and Guardant [11], all of whom are developing tests that identify multiple pieces of information from ctDNA and in some cases, other analytes.
Just like PinPoint, tests such as that being developed by GRAIL also use machine learning to analyse data and produce a probability of cancer; and just like PinPoint, all of these tests are sensitive to multiple cancers. The potential for ctDNA testing in future screening programmes is exciting but PinPoint addresses a more immediate problem faced by the NHS today: systemic overloading in cancer services and the lack of an affordable tool to accurately stratify patients at, or potentially before, the start of an urgent cancer referral.
Unlike many of our counterparts, PinPoint does not require investment in new physical infrastructure. Blood samples are processed using standard equipment in NHS labs and the algorithm exists within NHS IT systems for data security and ease of use. As a result, it can be adopted at high-speed and low-cost across regions.
The trend is clear: to get the most out of first-order testing, we need to apply new tools to an old process. A test like PinPoint can cut through the complexity of medical data to produce an accurate and repeatable result. This new generation of tests should give doctors extra confidence in their decision-making process. An algorithm will never replace a clinician but like any other medical device, it will answer questions and perhaps raise valuable new ones.
We live in an era where artificial intelligence, machine learning algorithms, and statistical models are increasingly able to offer insight and constructive support in the clinical space. After Deep Blue defeated Gary Kasparov in the late 90s, the best chess players weren’t computers, they were teams of humans using computers to help them. The chess-playing software became a useful tool and one that gave the human experts new perspectives to help them identify a more effective and successful route forwards.
This is a useful way of thinking about the new generation of blood test-based clinical decision support systems for cancer. They provide new sources of information for the trained clinical expert; they can support and enhance a doctor’s clinical intuition; they are new tools with which to diagnose and guide treatment for patients.
Far from being a threat to that vital human element in healthcare, the next generation of blood tests will be a powerful ally for doctors and patients alike.
For a full list of references, click here.
Who are PinPoint Data Science and how was the Test developed?
The PinPoint Test is a truly homegrown innovation. The company is based in the University of Leeds innovation hub, Nexus, and the collaboration between business, academia and the NHS that brought us to this point is a direct product of the fantastic health-tech ecosystem that exists in Leeds.
The company is led by CEO, Giles Tully; Executive Chair, Dr Nigel Sansom; Chief Scientist, Dr Richard Savage; COO, Dr Rosie Ferguson; CTO, Dr Matthew Neal; and CMO, Prof. Sean Duffy.
The Test itself was developed in collaboration with the University of Leeds and Leeds Teaching Hospitals NHS Trust, with support from the Leeds Academic Health Partnership, Yorkshire & Humber Academic Health Science Network, and West Yorkshire and Harrogate Cancer Alliance.

How did we get here?
To develop an algorithm like PinPoint’s, you first need high-quality data – a lot of it. PinPoint has collaborated with Professor Geoff Hall of Leeds Teaching Hospitals NHS Trust, who began developing an integrated digital care record for patients in Leeds in 2001. His ground-breaking work not only provides a platform from which clinicians can deliver improved personal care, but is also a source of uniquely detailed data with which to develop virtual tools.
As a result, we were able to complete a large- scale retrospective analysis of 371,799 patients from the Leeds region between 2011-2019, comprising development and validation sets of 224,669 and 147,130 patients respectively.
PinPoint Data Science and our collaborators from the NHS and University of Leeds have been published in BMJ Open, with a peer-reviewed paper entitled:
Preparing for rollout in the NHS
The PinPoint Test is currently undergoing a service evaluation run by the West Yorkshire and Harrogate Cancer Alliance. This is being used to confirm the performance of the Test in a real-world setting, to make sure it matches or exceeds the success of the retrospective analysis.
The evaluation is the final step before being able to deploy across wider regions of England, in preparation for which PinPoint Data Science received grants of over £1.7million from SBRI Healthcare and the NHS National Cancer Programme in 2022.
This means PinPoint is now working with AHSNs, Cancer Alliances and NHS Trusts in a total of five regions in England: West Yorkshire and Harrogate, Cheshire & Merseyside, Humber & North Yorkshire, Lancashire & South Cumbria, and Surrey & Sussex.
Together with these organisations, PinPoint is laying the foundations for widespread adoption of the Test, including quality assurance across laboratories and an implementation playbook to support a rapid roll-out. In addition, we are building educational tools for medical professionals and patients to better understand what a result from the PinPoint Test will mean and how it will inform but not dictate a pathway to diagnosis.
With the support of our partners in the NHS, the PinPoint Test should begin to become available for use in clinical decision-making in 2023.
Transformative Potential
COVID-19 brought into sharp focus the need for new solutions to old problems. The emergence of new technologies in machine learning and AI offers the opportunity to leverage these in creative new ways – reimagining the approach to cancer diagnosis and prioritising those at greatest risk. An all-new product like the PinPoint Test has the potential to transform the patient experience, reduce systemic overloading and allow clinicians to focus their time on the patients that need them most.
In October 2022, a peer-reviewed paper modelling the potential impact of the PinPoint Test on capacity at the Leeds Teaching Hospitals NHS Trust Breast Clinic was published by BMC.
The paper showed that PinPoint improved compliance with 2WW referral targets from approximately 66% to over 98%. Overspill appointments, where patients are forced to reschedule, were reduced by 50%. In addition, PinPoint reduced pressure on the pathway significantly enough that one ‘low-capacity clinic’ per week could be removed from the schedule entirely.
For more information, visit PinPoint at
www.pinpointdatascience.com