Lester Litchfield, Data & Science Manager at Volpara Health analyses how to build trust in the use of AI to improve and enhance breast imaging
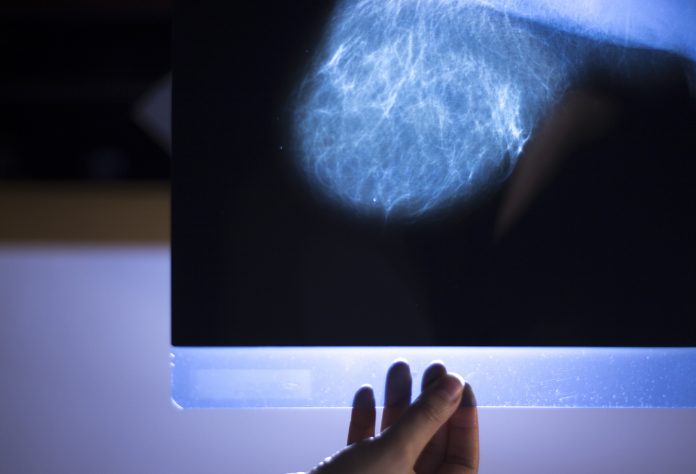
Artificial Intelligence (AI) has the potential to help increase early breast cancer detection and improve workflow management. AI can support automation of many repetitive tasks and management of large databases to enhance quality and reduce the workload in breast imaging.
Adoption of AI to enhance cancer detection has been slowed by the limited success of computer-aided detection (CAD) in the early 2000s. While the technology showed promise analysing mammograms in lab testing, it failed to deliver clear improvements when used in breast imaging clinics. At this point, trust in AI was uncertain. Over the years since, it became clear that for AI to succeed in breast care the quality and the rigour of the validation process needed to be at a much higher standard.
Fast-forward to 2021, companies such as Volpara are using AI to automate a range of tasks in breast imaging – from helping with U.S. Food & Drug Administration (FDA) quality audits to assessment of breast density. At the same time, AI and Deep Learning are pushing CAD to a level where prospective trials could determine conclusive benefits. (1) In addition, early indications suggest that new forms of AI are helping reduce reading times in 3D tomosynthesis. (2)
As countries around the world look for ways to improve and expand breast screening for more women, AI has an important role to help improve screening quality and cancer detection and contribute to personalisation and prevention. In an upcoming four-part series, we will examine key areas that can build trust in the use of AI to improve and enhance breast imaging such as:
- Optimising AI Acceptability in Clinical Practice.
- Performance/Quality Enhancement.
- Quantitative Breast Density to Inform Risk Assessment.
- Using AI to Predict and Prevent.
Optimising AI acceptability in clinical practice
As the first wave of AI in breast imaging, CAD did not meet clinical expectations, despite positive lab performance. In short, it appeared that the number of false positives generated by the AI overwhelmed readers to the extent that they would effectively ignore all the marks generated by the CAD software.
There are several ways to improve the acceptability of AI in clinical practice, some of which are being studied closely by regulators and other industry bodies around the world, and some of which are being practiced day in, day out by companies such as Volpara:
- Better training and testing over more diverse datasets (populations and machines).
- More prospective testing in independent settings.
- Making AI explainable.
Ultimately, the adoption of AI will depend on robust evidence of improved quality of patient care, increased efficiency, and cost-effectiveness, but trust and explainability are also key factors in getting clinicians engaged.
Practice performance and quality enhancement
Beyond clinical decision support, AI can be used to automate repetitive tasks, spot issues early, and to generate objective evidence for a variety of everyday tasks in breast imaging clinics. This is all done to keep quality high, but also to reduce costs and, importantly, stress on staff.
Volpara’s AnalyticsTM software is one such product and includes using AI to conduct a comprehensive assessment of mammography image quality, including positioning and compression and radiation doses. The FDA attributes poor positioning as the cause of most clinical image deficiencies today. The Analytics software provides automated and objective assessment of image quality on every mammogram by utilising a set of clinically validated algorithms that use x-ray physics and AI. Objectively assessing technologists’ patient positioning and resulting image quality provides technologists with continuous feedback and encourages ongoing performance improvements.
Breast density and risk assessment
As we move towards personalised screening strategies, there is starting to be agreement regarding how to gather, assess and act upon women’s risk factors. For example, the American College of Radiology (ACR) guidelines now recommend women receive a risk assessment at age 30, (3) but there have been suggestions from various groups to complete additional risk assessment later in life once a woman’s breast density is known from a mammogram which women typically start getting age 40 and up. (4) Breast density is a strong, independent risk factor for breast cancer. (5) Dense breasts are also very common among screening aged women (6) and is reported to contribute to a significant number of breast cancers in the population. (7)
A risk assessment incorporating breast density improves risk stratification and informs decisions about screening protocols.(8) Today, most radiologists rely on their own visual grading of breast density – a subjective and time-consuming process. High variability and inconsistencies have been found between radiologists (9) in contrast to automatic volumetric breast density software, which has shown good temporal consistency and reliability. (10,11) Subjective, inconsistent density scoring could result in insufficient screening protocols and sub-optimal patient outcomes.
Using AI to predict and prevent
The focus of most breast imaging today is early detection, but as risk prediction tools get better based on images and patient factors, we can foresee a world of prevention. Furthermore, once you’ve predicted who might develop breast cancer, you then need to apply preventative strategies and check that they are working. This monitoring of patients over time will help assess whether, for example, drugs to reduce cancer risk are changing the breast tissue in a way that is positive or potentially a risk. Imagine tracking the effects of hormone replacement therapy over time and flagging areas of concern.
Because of the variability in breast tissue, tracking and measuring change over time is a very difficult task. AI is well suited for this task if we can get diverse outcomes data based on millions (not just thousands) of women. This is what the power of AI and the Cloud – with the ability to store and process massive data – can enable. For example, Volpara currently has more than 50M mammograms stored in the Cloud from a wide mix of machines and people.
As breast cancer screening continues to transform to be more personalised and the paradigm shifts from early detection towards prevention, new uses of AI and the Cloud are emerging. The future of breast imaging is very bright, and AI and the Cloud are critical to that development.
Citations available upon request.
Please note: This is a commercial profile.
© 2019. This work is licensed under CC-BY-NC-ND.