A major clinical trial has found that low-dose interleukin-2 (IL2LD) is safe and may significantly extend survival in people with motor neurone disease (ALS)
Motor neurone disease affects around 45,000 people in Europe and attacks the nerves that control movement (motor nerves), so muscles no longer work. Around a quarter of people with the disease die within a year of developing symptoms, and more than half within two to three years of diagnosis.
The MIROCALS (Modifying Immune Responses and Outcomes in ALS) clinical trial found that interleukin-2 did not improve survival rates. Still, it did find a statistically significant survival benefit in about 80% of the study participants with a key biomarker.
Interleukin-2 helps regulate the immune system
Interleukin-2 is a molecule known to regulate the immune system in humans. The drug used in the trial, aldesleukin, is a manufactured human interleukin-2, which has been used in high doses in some cancers.
Low doses of interleukin-2 (IL2LD) have been found to reduce inflammation by increasing the number of white blood cells known as regulatory T cells (Tregs) in the blood. Previous studies have suggested that inflammation in the central nervous system is linked to an increased rate of progression of ALS/motor neurone disease and that increased numbers of Tregs are associated with better survival.
The drug reduced the risk of death in patients with Motor neurone disease
The MIROCALS trial recruited 220 people newly diagnosed with ALS/motor neurone disease, who were initially treated with riluzole (the standard treatment) before being randomised to receive either IL2LD or a placebo for 18 months.
The trial was double-blind to prevent participants and researchers from knowing which treatment participants were allocated. The researchers monitored safety and daily function. As the condition significantly shortened life, the primary measure of the effect of IL2LD at the end of the trial was survival.
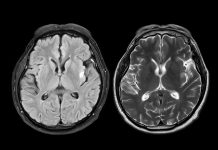
The researchers found the drug was safe with no excess side effects compared to the placebo. A primary analysis did not show a significant benefit for survival; however, a pre-planned, more detailed analysis taking into account the complexity of ALS revealed a statistically significant survival benefit in about 80% of the study participants who had lower levels of cerebrospinal fluid (CSF) phosphorylated neurofilament heavy chain protein (pNFH), a biomarker indicating the rate of motor neuron damage. In these people, the risk of death at the end of the study was reduced by over 40%.
Dr Gilbert Bensimon, MIROCALS study coordinator and principal investigator, stated: “ALS/MND is a complex disorder. The encouraging findings of the MIROCALS trial represent a significant step toward designing better trials and expediting the development of urgently needed treatments for ALS/MND. Importantly, IL2LD was safe and well-tolerated over a long period. Our findings underline the importance of the immune system as a target for treatments aimed at slowing the progression of this devastating condition.”
Professor Nigel Leigh, Chief Investigator and co-coordinator of the MIROCALS study and Neurology at BSMS, added: “This trial provides promising evidence that IL2LD benefits people with ALS/MND. The data, blood and CSF samples from the people who generously took part in the trial are now being used to advance our understanding of ALS and help the development of new therapies that can further slow disease progression and improve the lives of people living with ALS/MND. We are extremely grateful to The Motor Neurone Disease Association, The MyName’5 Doddie Foundation, MND Scotland, AFM-Téléthon France, and Association pour la Recherche sur la SLA, who have contributed to this ongoing work.”
Professor Timothy Tree, Professor of Immune Regulation and Immunotherapy at King’s College London and one of the study’s joint first authors, said, “These groundbreaking results offer the strongest evidence yet that targeting the immune system can make a real difference in the fight against this devastating disease. Thanks to the generosity of our trial participants, who donated vital samples, we are now conducting further research to understand better how the immune system drives disease progression and develop even more effective treatments.”