A new AI system developed at the University of Cambridge can analyse blood cell shapes with higher accuracy than human experts and detect abnormalities often overlooked by doctors, offering potential breakthroughs in diagnosing conditions like leukaemia
Researchers at the University of Cambridge have developed an AI tool that analyses the shape and morphology of blood cells, identifying abnormalities with greater precision than even expert haematologists. This innovation could transform the diagnosis of blood disorders, including leukaemia, by flagging subtle changes that doctors sometimes miss.
The results are reported in the journal Nature Machine Intelligence.
AI tool automates blood cell analysis to spot rare and abnormal cells
A research team has created a system called CytoDiffusion that uses generative AI to study the shape and structure of blood cells.
CytoDiffusion was developed by researchers at the University of Cambridge, University College London, and Queen Mary University of London and can accurately identify a wide range of regular blood cell appearances and spot unusual or rare cells that may indicate disease.
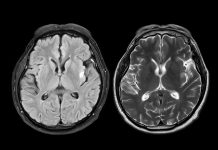
By identifying subtle differences in blood cell size, shape, and appearance, blood disorders can be diagnosed quickly. However, the task requires years of doctor training, and opinions can differ between professionals.
“We’ve all got many different types of blood cells that have different properties and different roles within our body,” said Simon Deltadahl from Cambridge’s Department of Applied Mathematics and Theoretical Physics, the study’s first author. “White blood cells specialise in fighting infection, for example. Knowing what an unusual or diseased blood cell looks like under a microscope is an important part of diagnosing many diseases.”
However, a typical blood ‘smear’ contains thousands of cells, far beyond what any human could analyse. “Humans can’t look at all the cells in a smear – it’s just not possible,” said Deltadahl. “Our model can automate that process, triage the routine cases, and highlight anything unusual for human review.”
“The clinical challenge I faced as a junior haematology doctor was that after a day of work, I would have a lot of blood films to analyse,” said co-senior author Dr Suthesh Sivapalaratnam from Queen Mary University of London. “As I was analysing them in the late hours, I became convinced AI would do a better job than me.”
Developing CytoDiffusion with AI
To develop CytoDiffusion, the researchers trained the system on over half a million images of blood smears collected at Addenbrooke’s Hospital in Cambridge. The dataset included both common blood cell types and rarer ones, as well as elements that can confuse automated systems.
By modelling the full distribution of cell appearances rather than just learning to separate categories, the AI tool can recognise rare or abnormal cells.
When tested, CytoDiffusion detected abnormal cells linked to leukaemia with far greater sensitivity than existing systems. It matched or surpassed current models, even when given far fewer training data, and quantified its own uncertainty.
“When we tested its accuracy, the system was slightly better than humans,” said Deltadahl. “But where it really stood out was in knowing when it was uncertain. Our model would never say it was certain and then be wrong, but that is something that humans sometimes do.”
“We evaluated our method against many of the challenges seen in real-world AI, such as never-before-seen images, images captured by different machines, and the degree of uncertainty in the labels,” said co-senior author Professor Michael Roberts, also from Cambridge’s Department of Applied Mathematics and Theoretical Physics. “This framework gives a multi-faceted view of model performance, which we believe will be beneficial to researchers.”
The results are promising, but the researchers note that CytoDiffusion is not a replacement for trained clinicians.
“The true value of healthcare AI lies not in approximating human expertise at lower cost, but in enabling greater diagnostic, prognostic, and prescriptive power than either experts or simple statistical models can achieve,” said co-senior author Professor Parashkev Nachev from UCL. “Our work suggests that generative AI will be central to this mission, transforming not only the fidelity of clinical support systems but their insight into the limits of their own knowledge. This ‘metacognitive’ awareness – knowing what one does not know – is critical to clinical decision-making, and here we show machines may be better at it than we are.”