Scientists have revealed how common variations in our blood cells can act as unexpected allies to cancer-causing mutations
This discovery, published in Nature Genetics, could reshape our understanding of how we develop these malignancies, potentially paving the way for better predictions and treatments.
What are myeloproliferative neoplasms?
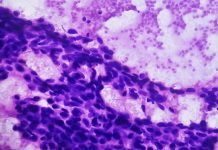
Myeloproliferative neoplasms (MPNs) are a group of chronic blood cancers affecting around 4,000 people in the UK each year. They occur when the bone marrow goes into overdrive, producing excessive blood cells.
This can lead to serious complications like blood clots, bleeding and even progress to other forms of cancer, like leukaemia. While scientists have pinpointed specific mutations in genes like JAK2 that can trigger MPNs, these mutations are surprisingly common in the general population.
Why don’t all carriers develop the disease?
This new study provides some answers; researchers from the Wellcome Sanger Institute and the University of Cambridge, led by DR. Jing Guo, combined data on these cancer-causing mutations with information on individual genetic variations that naturally influence blood cell traits.
The findings
These common, inherited variations, which determine things like our natural blood cell count, can play a crucial role in whether a JAK2 mutation leads to MPN.
“Our study shows that inherited variants can influence if a genetic mutation will go on to cause MPN,” explains Dr. Guo. “Individuals with an inherited tendency towards higher blood cell counts might be more susceptible to developing MPN features even without the cancer-driving mutations.”
This discovery has far-reaching implications. Firstly, it highlights why most people with the JAK2 mutation never develop MPN. Their inherited blood cell traits may act as a protective shield, preventing the mutation from taking hold.
Secondly, this knowledge could improve disease prediction. By factoring in the individual’s unique genetic makeup, doctors can more accurately assess their risk of developing MPN, ultimately leading to better clinical decisions and potentially reducing unnecessary interventions.
“Our hope is that this information can be incorporated into future disease prediction efforts,” says Dr. Jyoti Nangalia, co-senior author of the study. “This could help us identify individuals at higher risk and guide more personalized approaches to managing their health.”
How will this study help in the future?
This study is a significant step forward in our understanding of MPNs and, the complex interplay between our genes and disease development.
By considering cancer-causing mutations and the unexpected allies within our DNA, we can predict, prevent, and overcome these challenges better.