Lorna Rothery spoke to the Cancer Drug Development Forum’s Managing Director, Professor Jaap Verweij and Chairperson of the CDDF Board of Directors, Professor Ruth Plummer, about opportunities and challenges in oncology research and treatment
The Cancer Drug Development Forum (CDDF) is a non-profit organisation that fosters stakeholder collaboration to accelerate cancer drug development and treatment delivery. Part of its remit includes organising workshops, conferences, and webinars to bring stakeholders into a neutral space for productive dialogue; it works closely with regulators, researchers, pharmaceutical companies, and patient advocates. Lorna Rothery spoke to the CDDF’s Managing Director, Professor Jaap Verweij (JV) and Chairperson of the CDDF Board of Directors, Professor Ruth Plummer (RP), about the key milestones in oncology research and care, as well as the obstacles that need to be tackled to improve equitable access to cancer treatment and trials.
What have been some of the most significant milestones in improving cancer research and patient care across the EU since the CDDF was founded?
JV: The development of immunotherapy is likely the most significant breakthrough since the CDDF’s establishment in 2001. Additionally, introducing tyrosine kinase inhibitors has allowed for more focused treatments and enabled us to target the genetic mutations in tumours more directly.
RP: Immunotherapy and targeted agents have transformed the benefits for patients. The ability to do molecular profiling has also played a significant role in this transformation. In the UK and in some European countries, molecular profiling is now offered as a standard of care for patients going on trials. This approach has allowed us to provide optimised therapies to patients and avoid unnecessary toxicity to those for whom specific therapies may not be effective.
We now also have different classes of drugs available, such as small molecule inhibitors, monoclonal antibodies, and antibody-drug conjugates (ADCs).
Aside from COVID-19, what are the most pressing challenges facing cancer treatment and research?
RP: One of the main issues with cancer treatment in Europe and worldwide is the lack of equal access for all patients. The lack of equity in healthcare access is often caused by insufficient investment in economically disadvantaged areas. Resource shortages aside, the biggest challenge is ensuring everyone in Europe has equal access to treatment. This requires a collective effort from the community to address this issue.
When it comes to medical research, one of the major hurdles is adjusting and implementing recent regulatory changes effectively so that they do not lead to further inequity or delays across Europe. As someone who practices medicine in the UK, we face different challenges due to our decision to leave the EU in 2016. However, this does not mean we are not also affected by changing regulations. Hence, it is a collective issue for all of Europe.
Adapting to regulation changes is essential to keep clinical trials moving forward, but it’s challenging. Equitable access to trials generally is an issue, as they tend to be concentrated in a few locations, even within the same country. Regulators are pushing for more geographical diversity in the placement of trials, which is a step in the right direction. For example, it’s important to consider opening centres outside London in the UK. Similarly, there is a need to balance the distribution of trials across different regions of Europe; Western Europe tends to receive the bulk of trials, leaving the eastern parts of Europe behind.
The research space has abundant trials for patients with a given indication. There are not enough patients for every trial proposed, so there is a need to prioritise the right trials to answer the required research question and clear up clinical uncertainties. However, so many trials are available that ensuring recruitment of participants efficiently is challenging. It’s unclear how this issue
can be solved.
JV: Equity of healthcare access is closely linked to care affordability. Despite being a part of the EU, there are significant variations between countries in terms of the affordability of healthcare. The differences in these countries’ economies mean they have different options for paying for care. A significant concern is drug pricing; some drugs are too expensive for even the wealthiest countries to afford. This means that they are unavailable, as the cost of production outweighs the potential profit.
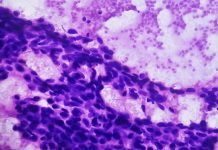
Advancements in biology have resulted in an overwhelming amount of information about diseases, leading to their fragmentation. When I was studying medical oncology, we recognised only four types of breast cancer; today, there are at least 30 different types, if not more. This makes conducting clinical trials more challenging and complex, often requiring multi- country or multi-continent studies.
Europe’s pharmaceutical industry is lagging behind that of the United States, which is evolving quickly. Most large pharma companies are now based in the US and prioritise focusing on the biggest market, the US market. As a result, they are focusing less on Europe and elsewhere, a trend that may not benefit European patients and those in Asia Pacific and other regions. Although this has not yet become a reality, there is a growing tendency among pharma companies to consider this expansion.
RP: In Europe, patients who participate in dose-finding safety studies have typically received fewer lines of treatment and are less heavily pretreated than US patients due to differences in healthcare systems. Because of this, we may get differences in the fitness of a patient, and their ability to undergo treatment. This and genetic differences between populations can end up meaning that effective recommended doses may be different. At present, the concentration of large pharma headquarters in the US, means many more studies are doing initial dose finding in the US only.
How can regulation of clinical research and data evolve to better support patient-friendly innovation?
RP: To be patient-friendly, we need to learn to work collaboratively. This requires continuing dialogue with regulatory bodies and the establishment of consistent regulations across Europe, including the UK. By doing so, we can eliminate the need for each country to evaluate trial data separately. While some country-specific aspects may need to be considered, generally, what is safe and right in one country will be so in another. This would ultimately benefit patients by streamlining the process and ensuring consistency.
Safe data sharing and creating secure research data environments are crucial. In my experience, patients are willing to share their data if they know it may benefit others and they trust that their data won’t be misused. Countries like the Netherlands and the UK have national healthcare systems with increasingly digitalised hospitals, which makes data collection and sharing easier. This data can be curated to be anonymised. Real-world data is becoming a valid way of generating information, and will be considered as such by regulators especially regarding rarer types of cancers. An extensive patient data collection on standard care treatment could be incredibly valuable in assessing improvements in care. Consortiums like the PRIME-ROSE Consortium in Europe are making considerable efforts to create a secure and safe data-sharing environment. We will eventually get there, and it will be a significant benefit.
JV: To protect patient privacy and ensure data accuracy, we have created complex laws causing confusion and slowing down the process of conducting trials, collecting data, and submitting it to the appropriate regulatory bodies. We have become too focused on protecting ourselves and over-regulating, which is ineffective. Although regulations are necessary, we must use common sense and simplify the process. In a recent workshop, the in vitro diagnostics regulation of the European Union was identified as a significant obstacle to conducting studies in Europe. Two-thirds of studies are still being conducted overseas, and one-third are no longer being performed in Europe due to this regulation. This prevents patients from accessing potentially life-saving treatments and needs to be addressed. However, there is no clear solution to this problem at the moment.
How is the CDDF working to support and accelerate cancer drug development?
JV: At the CDDF, we have various stakeholders, including patient advocacy groups, regulators, academia, and the pharmaceutical industry. When we talk about regulators, we should note that some approve new dossiers while others approve drugs for actual use, known as a health technology assessment. This is crucial for patient access in individual countries. Our goal is to gather different people who have different perspectives on a particular topic and engage them in a debate. We aim to find common ground and work together to find a solution that benefits everyone. Of course, it’s not possible to find a solution in just one two-day workshop. However, we can make changes over time by implementing a repetitive system. What’s great is that regulators are also involved, which is a fantastic asset because it means we can incorporate their opinions and ensure that everyone is happy with the new direction we’re taking.
In 2015, an accelerator platform was established in pediatric oncology. The CDDF brought forward this initiative, which was later taken over by pediatric oncology societies. The goal was to accelerate drug development for children with cancer, which is even more difficult than developing treatments for adults, and clinical trials are more challenging to conduct. The platform has played a crucial role in pushing things forward.
RP: Most of us on the board are clinical academics, and some are ex-regulators or patient group members, but we act as private individuals to ensure impartiality. Our role is to organise the workshops in collaboration with stakeholders, but we remain neutral.
Looking to the future, where do you believe the next breakthrough in cancer drug development will lie?
RP: A game changer in cancer treatment would be the ability to make cellular therapies work in solid tumours as they do in hematologic malignancies. If this is achieved, it would mean a one-time treatment that could potentially cure cancer. However, it is proving to be a challenge due to associated toxicity. Surgery does cure a lot of patients if the cancer is found early. However, while new systemic cancer treatments are used to treat the disease, in the majority of patients cancer cells eventually evolve, become resistant and require another treatment. Thus, the ability to have a one-time cure treatment would completely change the cancer care model. These treatments are coming, but equity of access is a huge issue because they require highly specialised hospitals and are expensive. If they can be made accessible to more people, it would be a game- changing moment for cancer care.
JV: This would change the financial model for cancer care; if you have a very effective treatment that could cure everyone, you could, in theory, spread the cost of that treatment over many years.
The Cancer Drug Development Forum (CDDF)
Tel: +32 2 880 62 70
info@cddf.org
https://cddf.org
Twitter
LinkedIn
Contributor Details
Editor's Recommended Articles
-
Must Read >> Advocating for equity in childhood cancer care