Around 1,500 people in England with multiple myeloma will benefit from belantamab mafodotin, used in combination with bortezomib and dexamethasone
Multiple myeloma is a long-term, incurable cancer of the blood plasma cells that goes through periods where symptoms worsen (relapse) and periods where treatment brings the disease under control (remission). People with the condition can experience debilitating complications such as frequent infections and kidney problems that severely impact their quality of life.
New guidance from NICE recommends this treatment for adults with multiple myeloma who have had one previous treatment containing lenalidomide, and who either cannot tolerate lenalidomide or whose cancer has become resistant to it.
“We’re delighted that people in England will become among the first in the world to access belantamab mafodotin for this indication. This recommendation demonstrates our commitment to getting the best care to patients fast while ensuring value for the taxpayer,” said Helen Knight, director of medicines evaluation at NICE.
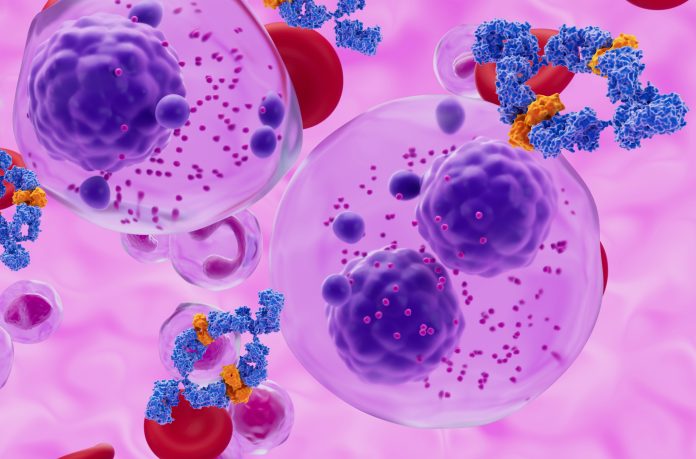
Targeted therapy for multiple myeloma
Belantamab mafodotin works by specifically targeting a protein called BCMA, which is found in myeloma cancer cells. The antibody part binds to and attaches to cancer cells, while the drug part delivers cancer-killing medicine directly to these cells.
This treatment is the only one of its kind available for multiple myeloma, offering patients a new option to treat their cancer once other treatments have stopped working.
Belantamab mafodotin is administered via infusion in combination with bortezomib (given as an injection) and dexamethasone (typically taken as tablets).
The three-year survival rate of 74% belantamab mafodotin trial
The new clinical trial, called DREAMM-7, showed that a combination of belantamab mafodotin, bortezomib, and dexamethasone (BVd) significantly improves outcomes for patients with relapsed or refractory multiple myeloma compared to the standard regimen of daratumumab, bortezomib, and dexamethasone (DVd).
Among 494 patients enrolled, those receiving BVd had a median progression-free survival (PFS) of 36.6 months, nearly three times longer than the 13.4 months seen with DVd. At 18 months, overall survival was 84% in the BVd group compared to 73% in the DVd group. Additionally, 25% of patients on BVd achieved a complete response or better, with no minimal residual disease, compared to just 10% in the DVd group.
However, the enhanced efficacy came with a higher rate of adverse events. Grade 3 or higher side effects occurred in 95% of BVd patients, and eye-related issues were reported in 79%, though most resolved with dose adjustments.
These results support BVd as a promising new option for patients with relapsed or refractory multiple myeloma and may influence future treatment guidelines.
Professor Peter Johnson, NHS England’s National Clinical Director for Cancer, said: “Myeloma is an aggressive type of blood cancer, but we have seen a steady improvement in the outlook for patients over recent years as we have introduced new targeted therapies.
“I am delighted that patients in England will be the first to benefit from this new treatment, which has the potential to keep cancer at bay for years longer, giving people the chance of more precious time with friends and family.
“This treatment could be life-changing for many patients and their families, and that’s why it is so important that the NHS continues to secure quick access to the latest, innovative treatments like this, at affordable prices to the taxpayer.”
Health Minister Karin Smyth said: “This groundbreaking therapy puts the NHS at the forefront of cancer innovation. By harnessing cutting-edge ‘trojan horse’ technology, we’re offering new hope to blood cancer patients across the country.
“We’re determined to back scientific breakthroughs that deliver real results for patients – bringing the latest treatments from the lab to those who need them most. It’s another example of how we’re building an NHS fit for the future, one that embraces medical innovation to transform patient care.”
Shelagh McKinlay, Director of Research and Advocacy at blood cancer charity Myeloma UK, said: “It’s fantastic to see the UK at the forefront of myeloma treatment. NHS England has demonstrated that myeloma patients can have world-first access to innovative drugs.
“We have been working very hard for the last year to get this treatment approved, and we know it will transform the lives of thousands of people with myeloma.”