Asal Shirazi BEM, the Founder and CEO of ASA Foundation, shares insights into how inflammatory mechanisms drive autoimmunity and highlights the role of environmental toxins, along with effective strategies to mitigate their impact
Inflammation is an essential host defence that becomes pathogenic when dysregulated. Chronic, systemically amplified inflammation underpins the initiation and progression of many autoimmune diseases through loss of tolerance, cytokine pathway imbalance, and self-sustaining tissue damage. Increasingly, environmental exposures – including air pollution and endocrine-disrupting chemicals (EDCs) – are implicated as triggers that potentiate inflammatory networks, alter the microbiome, and tilt genetically susceptible individuals toward autoimmunity. This review summarises contemporary evidence (2023–2025) on inflammatory mechanisms in autoimmunity and the roles of environmental toxins as upstream drivers, with brief notes on mitigation strategies.
Acute inflammation confines injury and promotes repair; by contrast, chronic inflammation drives persistent cytokine activation, lymphocyte dysfunction, and progressive tissue injury. Autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus (SLE), multiple sclerosis, psoriasis, and autoimmune thyroid disease exemplify this maladaptation. Recent literature refines our understanding of pro-inflammatory cytokine axes (e.g., IL-6, IL-17/Th17) in autoimmunity and highlights environmental exposures – especially fine particulate matter (PM₂.₅) and EDCs – as causal or contributory risks for disease onset and flares. (1–6,9–12)
Inflammatory mechanisms in autoimmunity
Loss of immune tolerance emerges from convergent defects in regulatory T-cell function, antigen presentation, and innate sensing, culminating in pathogenic cytokine circuits. IL-6 is a pleiotropic cytokine essential to acute responses; its dysregulation sustains chronic inflammation and has validated therapeutic targeting (e.g., IL-6 receptor blockade) in inflammatory arthritis. (1) Parallel advances implicate Th17 cells and the IL-17 family across multiple autoimmune diseases – including MS, IBD, psoriasis, and spondylarthritis – where IL-17 signalling amplifies neutrophil recruitment, barrier dysfunction, and tissue damage. (2,3) More broadly, pro- and anti-inflammatory cytokine balance (‘cytokine rheostat’) is now recognised as a determinant of disease trajectory and treatment response. (1–3)
Environmental triggers: air pollution
Epidemiologic and genetic-instrumental studies increasingly link long-term PM₂.₅ exposure to autoimmunity. A 2024 Mendelian randomisation analysis reported a causal association between PM₂.₅ and psoriasis in European populations, supporting a mechanistic role for pollution in inflammatory skin autoimmunity. (4) In 2025, a prospective Taiwanese cohort found higher incident SLE risk with increased PM₂.₅ exposure, reinforcing temporality and dose–response features in a systemic autoimmune context. (5) Complementing these, a 2025 synthesis indicates that even ‘relatively low-level’ ambient air pollution may elevate autoimmune risk, underscoring that current exposure standards may not be fully protective for susceptible groups. (6) Mechanistically, inhaled particulates generate oxidative stress, activate innate immune sensors (e.g., inflammasomes, TLRs), disrupt epithelial barriers, and propagate systemic cytokine signalling, thereby lowering the threshold for autoimmunity in genetically predisposed individuals. (1,4–6,12)
Environmental triggers: endocrine-disrupting chemicals
EDCs – including bisphenols, phthalates, dioxin-like compounds, and certain pesticides – interfere with hormone action and immune regulation. A 2023 narrative review synthesised evidence that EDC exposure perturbs immune signalling and promotes autoimmune phenomena across organ systems. (7) Focused updates in 2025 highlighted associations between EDCs and autoimmune thyroid disease (AITD), with mechanistic links spanning oestrogen receptor cross-talk, oxidative stress, and epigenetic modifications that bias toward pro-inflammatory phenotypes. (10) Position statements and risk assessments continue to emphasise the breadth of EDC sources and the plausibility of low-dose mixture effects on endocrine–immune axes relevant to autoimmunity. (9) Collectively, these data support precautionary exposure reduction, particularly for individuals with autoimmune susceptibility.
The microbiome as a mediator
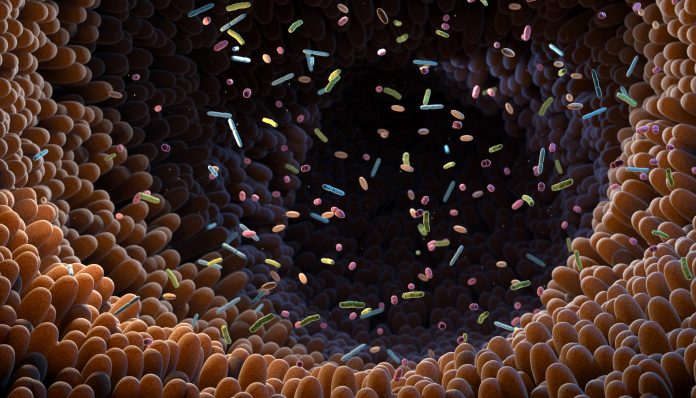
Dysbiosis bridges environmental exposure and immune dysregulation. A 2024 review outlined mechanistic routes by which altered gut communities drive aberrant Th17 differentiation, impaired Treg function, and molecular mimicry, thereby fostering autoimmune pathways. (8) In 2025, a meta-analytic synthesis across autoimmune neurological disorders reinforced consistent dysbiosis patterns and suggested biomarker potential for diagnosis and therapeutic monitoring. (11) These findings align with the concept that toxins and air pollutants can reshape gut ecology, increase intestinal permeability, and escalate systemic immune activation. (8,11,12)
Integrative model: genes, inflammation, and the exposome
Autoimmunity emerges from gene–environment interactions rather than genetics alone. Contemporary frameworks integrate HLA and non-HLA susceptibility with the ‘exposome’ – the totality of environmental exposures over time – where pollutants and EDCs act as inflammatory catalysts that unmask or accelerate disease in predisposed hosts. (12) The convergence on Th17/IL-17 and IL-6 axes across diseases provides a mechanistic scaffold linking diverse exposures to shared inflammatory endpoints. (1–3,8)
Mitigation and clinical implications
Exposure reduction: practical steps include limiting PM₂.₅ exposure (ventilation/filtration, high-pollution day avoidance), minimising plastics/contact with known EDC sources, and adopting lower-toxin personal/home products. Given signals that ‘low-level’ exposures confer risk, a conservative approach is justified for vulnerable patients. (6,7,9,10)
Microbiome-supportive care: diets rich in fibre and polyphenols, prudent antibiotic use, and evidence-based probiotics/prebiotics may help restore immune balance, though disease-specific RCTs remain needed. (8,11)
Targeted anti-inflammatory therapy: biologics and small molecules aimed at IL-6, IL-17/Th17, JAK–STAT, and related pathways can quell pathogenic inflammation; aligning pharmacotherapy with exposure reduction may optimise outcomes. (1–3)
Public health policy: emerging causal evidence linking air pollution to autoimmunity argues for tighter air-quality standards and EDC regulation to reduce population-level inflammatory burden. (4–6,9,10)
Chronic, dysregulated inflammation is the engine of autoimmune pathology. New evidence strengthens causal links between environmental exposures – particularly PM₂.₅ and EDCs – and autoimmune risk, likely mediated by oxidative stress, barrier injury, innate immune activation, cytokine imbalance, and microbiome disruption. Clinicians and patients can act now by pairing targeted anti-inflammatory therapies with pragmatic exposure mitigation and microbiome-supportive strategies, while advocating for policy reforms that address upstream drivers.
References
- He Y, Burmester GR, et al. Pro- and anti-inflammatory cytokines: the hidden keys to immune homeostasis and targets for therapy. Front Pharmacol. 2024;15:1450558.
- Lee YK, Kim KW, et al. Th17 cell pathogenicity in autoimmune disease. Exp Mol Med. 2025;57
- Zhao X, Li J, et al. Role of Th17 and IL-17 cytokines on inflammatory and autoimmune diseases: therapeutic implications. Int J Mol Sci. 2023;24(18)
- Hu H, Wang J, et al. Causal association between PM₂.₅ and psoriasis: a Mendelian randomization study in Europeans. Front Public Health. 2024;12:1333811.
- Lai Y-J, Lin C-Y, et al. Higher PM₂.₅ exposure increases the risk of incident systemic lupus erythematosus: a prospective cohort study in Taiwan. Ann Rheum Dis. 2025.
- Leng R-X, Pan H-F, et al. The impact of relatively low-level ambient air pollution on autoimmune diseases: current evidence and challenges. Autoimmun Rev. 2025
- Huang RG, Xu Y, et al. Endocrine-disrupting chemicals and autoimmune diseases: current evidence and mechanisms. Environ Res. 2023;231:116071.
- Sai A, Vohra S, et al. Influence of gut microbiota on autoimmunity: mechanistic insights and therapeutic prospects. J Transl Autoimmun. 2024;7:100175.
- Endocrine Society. Endocrine-Disrupting Chemicals—2024 update (position statement draft for comment). 2024.
- Monaghan M, et al. Endocrine-disrupting chemicals and autoimmune thyroid disease: a systematic review. Best Pract Res Clin Endocrinol Metab. 2025;xx:xxxx–xxxx.
- Deng X, Li Y, et al. Perturbations in gut microbiota composition in autoimmune neurological disorders: a systematic review and meta-analysis. J Neuroimmunol. 2025;xx:xxxx–xxxx.
- Touil H, et al. Differential impact of environmental factors on systemic autoimmunity: mechanisms and clinical implications. Front Immunol. 2023;14:1147447.