UCL researchers have developed an ultrasound helmet that enables deep brain stimulation without surgery, offering hope for Parkinson’s and other neurological disorders
Researchers at University College London (UCL), in collaboration with the University of Oxford, have introduced a groundbreaking ultrasound helmet capable of non-invasively stimulating deep brain regions. This advancement marks a significant step forward in neuromodulation technology, providing a potential alternative to traditional surgical interventions for neurological conditions such as Parkinson’s disease.
The study is published in Nature Communications.
From Transcranial ultrasound stimulation to non-surgical deep brain stimulation
Looking for a way to modulate brain function is a key research area that scientists are trying to break. Transcranial ultrasound stimulation (TUS) is one technology poised to challenge our understanding of how the brain works and treat neurological diseases. It works by modulating the activity of neurons by delivering gentle mechanical pulses that influence how the cells send signals.
However, this type of technology has struggled to reach deeper brain areas with sufficient precision to target specific brain structures, often targeting broader regions, which limits its use for targeted neuromodulation.
Researchers have now introduced a new ultrasound device capable of deep brain stimulation and influencing deep brain regions without the need for surgery for the first time. This device targets areas approximately 1,000 times smaller than conventional ultrasound devices can pinpoint and 30 times smaller than previous deep brain ultrasound devices.
Researchers found lasting changes in brain function
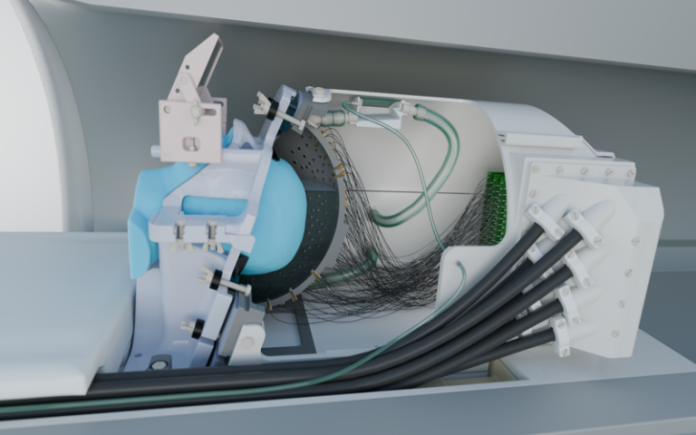
The new non-surgical deep brain stimulation device features 256 elements configured within a specialised helmet to send focused beams of ultrasound to specific parts of the brain, allowing for the modulation of neuronal activity. It also includes a soft plastic face mask, which helps to target the ultrasound waves more precisely by keeping the head still.
The researchers used deep brain stimulation technology on seven human volunteers, targeting a part of the thalamus, a small structure in the centre of the brain that helps relay sensory and motor information, specifically the lateral geniculate nucleus (LGN). The LGN is involved in processing visual information.
The first experiment saw participants watching a flashing checkboard, which sent signals to the brain through the eyes. During the stimulation with the ultrasound device, a functional magnetic resonance imaging (fMRI) scan showed significantly increased activity in the participants’ visual cortex, confirming precise targeting of the LGN. The second experiment revealed sustained decreases in visual cortex activity for at least 40 minutes after ultrasound stimulation, highlighting the system’s potential for inducing lasting changes in brain function.
Though participants did not consciously perceive any changes in what they were seeing during the experiments, the brain scans revealed significant changes in neural activity. The ultimate goal is to harness these effects to produce clinically beneficial outcomes, such as stopping hand tremors.
New hope for Parkinson’s disease and other neurological conditions
Deep brain stimulation requires invasive surgery and carries associated risks. However, the new ultrasound system, which utilises deep brain stimulation technology, is non-invasive and offers comparable precision.
The researchers will carry out further studies to fully understand the mechanisms underlying TUS-induced neuromodulation. However, the initial findings highlight a significant milestone in the development of safe, effective, and targeted brain stimulation technologies.
Professor Bradley Treeby, senior author of the study from UCL Medical Physics and Biomedical Engineering, said: “This advance opens up opportunities for both neuroscience research and clinical treatment. For the first time, scientists can non-invasively study causal relationships in deep brain circuits that were previously only accessible through surgery.
“Clinically, this new technology could transform the treatment of neurological and psychiatric disorders like Parkinson’s disease, depression, and essential tremor, offering unprecedented precision in targeting specific brain circuits that play key roles in these conditions.
“The ability to precisely modulate deep brain structures without surgery represents a paradigm shift in neuroscience, offering a safe, reversible, and repeatable method for both understanding brain function and developing targeted therapies.”
Dr Eleanor Martin, first author of the study from UCL Medical Physics and Biomedical Engineering, said: “We designed the system to be compatible with simultaneous fMRI, enabling us to monitor the effects of stimulation in real time. This opens up exciting possibilities for closed-loop neuromodulation and personalised therapies.”
Dr Ioana Grigoras, a first author of the study from the Nuffield Department of Clinical Neurosciences, University of Oxford, said: “This novel brain stimulation device represents a breakthrough in our ability to precisely target deep brain structures that were previously impossible to reach non-invasively. We are particularly excited about its potential clinical applications for neurological disorders like Parkinson’s disease, where deep brain regions are especially affected.”