Gail Dianne Lewis, the Senior Principal Scientist at Discovery Oncology Genentech, Inc. analyses the human epidermal growth factor receptor 2
Human epidermal growth factor receptor 2 (HER2, ErbB2) was identified in 1985 through its close homology to the human epidermal growth factor receptor, EGFR (1). EGFR and HER2 are receptor tyrosine kinases comprised of extracellular, transmembrane, and intracellular domains, the latter possessing tyrosine kinase activity.
The oncogenic potential of HER2
The oncogenic potential of HER2 was demonstrated through transformation assays and the promotion of tumor growth in immunodeficient mice (2). Importantly, oncogenic transformation was evident only in cells that overexpressed HER2. Probes for detecting HER2 were subsequently used for analysing HER2 gene expression in human breast cancer (BC) samples. HER2 gene amplification was detected in approximately 20% of BC and, importantly, correlated with reduced survival (3,4). These findings led to considerable efforts to develop therapeutics to target HER2. The accessibility of the HER2 extracellular domain on the tumor cell surface renders HER2 an ideal candidate for antibody-based therapeutics.
A panel of HER2-specific monoclonal antibodies was generated at Genentech (5) and tested on a panel of cancer cells. Like the clinical findings, HER2 was overexpressed on a subset of human breast and ovarian cancer cells. Moreover, treatment with HER2 antibodies inhibited tumor cell growth only in cells which overexpressed HER2 (6). The most potent antibody, 4D5, was humanized (7) for use in patients and was designated trastuzumab (Herceptin®).
Humanization reduces immunogenicity of mouse antibodies and allows interaction of the antibody Fc with Fc receptors on immune cells to mediate antibody-dependent cellular cytotoxicity (ADCC).
Clinical development of trastuzumab
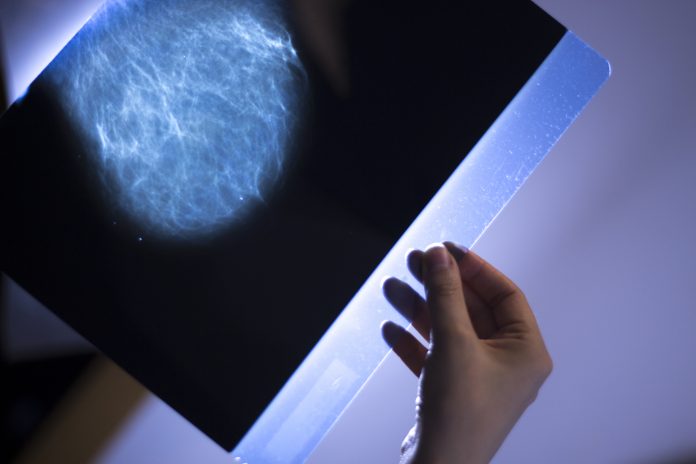
Because HER2 expression correlated with preclinical anti-tumor activity, a companion diagnostic for HER2 expression was included for clinical testing of trastuzumab. The importance of this cannot be understated, as clinical trials in unselected patients would likely have been negative.
The registrational trial demonstrated that trastuzumab combined with either taxane or anthracycline chemotherapy improved response rates and survival compared to chemotherapy alone as first-line treatment in patients with HER2-positive metastatic BC (8). Based on these findings, trastuzumab was approved by the US FDA in 1998. The clinical activity of trastuzumab/ chemotherapy was subsequently tested in the adjuvant setting, showing significant improvement in invasive disease-free survival compared to chemotherapy (9, 10). Trastuzumab is routinely used for neoadjuvant, adjuvant, and first-line treatment inpatients with HER2-positive BC, as well as in later lines of treatment in patients whose disease progresses.
Pertuzumab blocks HER2 dimerization with other HER/ErbB receptors
Investigation into the biology of the HER/ErbB family of receptors and ligands continued after the discovery of HER2. Prior to this, ligands for EGFR had been identified. Upon discovery of HER3 and HER4 receptors, (11, 12), the neuregulins/heregulins were identified as ligands for HER3 and HER4 (13). Although HER2 has no known ligand, it is the preferred dimerization partner for the other HER/ErbB receptors.
In particular, the HER2-HER3 complex transduces the most potent signals for cell proliferation and survival (14). These discoveries were instrumental in understanding the mechanism of a different HER2 antibody, 2C4/pertuzumab/Perjeta®, from the original hybridoma panel. Pertuzumab binds the dimerization arm of the HER2 extracellular domain (subdomain II), in contrast to trastuzumab, which binds subdomain IV (15).
In the presence of growth factors, which activate receptor dimerization, pertuzumab blocks HER2 dimerization with other HER receptors, inhibiting growth factor-stimulated downstream signalling. Like trastuzumab, pertuzumab mediates ADCC. The distinct and overlapping mechanisms of action led to clinical studies investigating pertuzumab with trastuzumab/chemotherapy. Results from neoadjuvant (NeoSphere; 16) and first-line (CLEOPATRA; 17) trials demonstrated significantly improved pathological complete response rates and overall survival upon the addition of pertuzumab, leading to approval in these indications. Pertuzumab was later approved in the adjuvant setting in patients with HER2-positive early BC in a subset of patients with high risk for disease recurrence (10).
Small molecule inhibitors of HER2
In addition to antibody therapy, small molecule inhibitors of the HER2 tyrosine kinase were developed. Lapatinib/ (Tykerb®), a HER2/EGFR kinase inhibitor is approved for HER2- positive metastatic BC in patients who have received prior trastuzumab and chemotherapy (18). Neratinib (Nerlynx®) is an irreversible pan-HER inhibitor approved for extended adjuvant therapy following trastuzumab-based treatment (19) and in combination with capecitabine for HER2-positive metastatic BC patients who received more than two prior anti-HER2 therapies (20). Tucatinib (Tukysa®), a HER2-selective tyrosine kinase inhibitor, was approved in combination with trastuzumab and capecitabine for patients with HER2-positive metastatic BC, including brain metastases, who had received one or more prior anti- HER2-based treatments (21). Importantly, a significant improvement in survival was demonstrated in patients with brain metastases in the tucatinib arm.
Antibody-drug conjugates for HER2-positive breast cancer During the past decade, antibody-drug conjugates (ADCs) have emerged as highly active agents in human cancer. ADCs are comprised of an antibody linked to a cytotoxic agent, leveraging the tumor selectivity of the antibody to deliver the cytotoxic to cancer cells. The first HER2 ADC developed was trastuzumab emtansine (T-DM1, Kadcyla®), utilizing trastuzumab covalently linked to DM1, an anti-mitotic agent, through a non-cleavable linker (22). T-DM1 demonstrated robust activity in trastuzumab-sensitive and – insensitive preclinical models of HER2- positive BC. T-DM1 was first approved in 2013 for the treatment of patients with HER2-positive metastatic BC after prior treatment with trastuzumab and a taxane (23).
In 2019, T-DM1 received approval for adjuvant treatment of early HER2- positive BC patients who have residual disease following neoadjuvant therapy (24). Following the success of T-DM1, several HER2 ADCs entered preclinical and clinical development. Of these, the only other HER2 ADC currently approved is trastuzumab deruxtecan (T-DXd, Enhertu®). Like T-DM1, trastuzumab is the antibody backbone of T-DXd. However, in T-DXd trastuzumab is linked to a topoisomerase 1 inhibitor using a protease cleavable linker (25). Moreover, there are more drugs linked to trastuzumab in T-DXd (drug-antibody ratio, DAR, of ~8) vs. T-DM1 (DAR ~3.5). These differences in ADC components afforded T-DXd improved clinical activity compared to T-DM1 when tested in the second-line setting (26), leading to the approval of T-DXd in this patient population.
In addition to antibodies, kinase inhibitors and ADCs, other modalities are under exploration for HER2-positive BC. These include vaccines, bispecific antibodies and cell therapies (27). The cloning and characterization of HER2 more than 30 years ago, along with the identification of the oncogenic role of HER2 in BC, resulted in the development of highly effective treatments that have prolonged the lives of many BC patients. Despite these advances, survival and cure rates can still be improved. It is the hope that some of the current and new treatment modalities will provide additional benefits to patients with HER2-positive BC.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.