Josep Figueras and Anna Sagan from the European Observatory on Health Systems and Policies focus here on antimicrobial resistance and ponder whether or not this could be the next big pandemic
The sudden emergence of the COVID-19 pandemic brought the world to its knees in 2020. To date, over 800,000 people across the globe have succumbed to the deadly virus and, sadly, the count keeps on rising. With national economies plunging into contractions following many weeks of lockdowns, the full societal cost of the pandemic is yet to unravel.
Despite the existence of International Health Regulations (IHRs), national pandemic preparedness plans, and some high-profile warnings in recent years, COVID-19 has caught us all largely off guard.
After over nine months since the first case was reported, the virus remains present in most countries around the world and uncontrollable in some. With children back at schools and with health systems in the northern hemisphere preparing for the winter influenza season, it is unsurprising that COVID-19 continues to captivate the attention of the general public and public decision-makers alike.
The danger of antimicrobial resistance
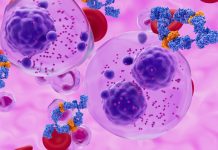
Yet, there are other challenges that we must not forget about. Antimicrobial resistance (AMR) is one of the urgent global health challenges of our times. AMR is the natural ability of microorganisms such as bacteria to become resistant to antimicrobial medicines. This Darwinian ability has always been present, and, in the past, we have responded to it by developing novel antibiotics and other antimicrobials. However, as global consumption of antibiotics in both humans and animals has increased and the antibiotic pipeline has dried up, AMR has increasingly put modern medicine under threat. In the relatively near future, AMR may render operations as easy as a wisdom tooth extraction, let alone hip replacement, organ transplant or cancer chemotherapy, impossible. The consequences of this may potentially be more severe and more difficult to contain than that of COVID-19.
Can AMR be mitigated?
Drug-resistant diseases already claim at least 700,000 lives globally and this number is estimated to rise to 10 million deaths each year by 2050 if no action is taken. In the EU alone, AMR causes the estimated death of 33,000 individuals every year and costs the bloc about €1.5 billion per annum in healthcare costs and productivity losses.
However, this burden can be reduced significantly by implementing effective intersectoral policies. A recent report by the Organisation for Economic Co-operation and Development (OECD) and the European Centre for Disease Prevention and Control (ECDC) review policies that are currently in place and show how this can be achieved affordably and cost-effectively. AMR is a threat we know and can mitigate.
But unlike COVID-19, the danger of AMR has been creeping up on us silently and gradually and it has taken time for the seriousness of this threat to trickle down to the public consciousness. Further, the complexity of the problem and the need for an integrated response across human, animal and environmental sectors can prove challenging. In many countries, AMR is still perceived more as a human health problem and there is insufficient coordination across sectors. Yet, international and national efforts to combat AMR have increased substantially over the past two decades, and a number of important positive developments can be noted.
The fight against AMR in Europe and beyond
Already in 1998, the European Commission established the European Antimicrobial Surveillance System (EARSS). In 2011, the Commission issued a “Communication on an Action Plan against the rising threats from AMR” and also in the same year, Member States of the WHO European Region adopted the European Strategic Action Plan on AMR. The Communication was later updated by the adoption of the 2017 “EU One Health Action Plan against AMR”, which aims to make the EU a best practice region, boost research, development and innovation, and shape the global agenda. Over the years, the Swedish, Danish, Dutch and most recently the Romanian presidencies of the EU Council have provided important platforms to advocate for EU-wide action against AMR.
Going beyond Europe, fight against AMR gained much momentum with the launch of the World Health Organization (WHO) Global Action Plan on AMR in 2015, which asked all countries to develop national action plans (NAPs) by 2017. The second landmark development was the United Nations (UN) General Assembly political declaration in 2016 where countries committed to develop and implement multisectoral NAPs across human, animal and environmental health in accordance with the ‘One Health’ approach. This approach recognises that the roots of AMR are multifaceted and interconnected and that while using fewer antibiotics in humans is critical to reducing resistance, factors such as agricultural activity, industrial pollution and other environmental influences should also be addressed. Since the dominant drivers will differ in various contexts, locally driven NAPs are paramount to success in the fight against AMR.
AMR: More public and private action is needed
Countries around the world have been using NAPs as the best way to build engagement among stakeholders and coordinate a range of actions across human, animal and environmental health. Yet, in spite of most countries already having or developing a NAP, even in more developed countries such as in the EU/EEA region, implementation of NAPs varies significantly. For example, many of the NAPs lack an operational or monitoring plan and only a fifth of EU/EEA countries have a multisectoral NAP with identified funding sources.
Other efforts, such as stimulating R&D into novel antimicrobials, vaccines and rapid point-of-care diagnostics, remain inconsistent across countries and inadequate on a global scale. For example, despite the repeated endorsement of incentives such as the market entry rewards (MERs) to stimulate R&D in antibiotics, no nation has so far taken the lead in establishing a fund to finance such a scheme.
Important initiatives have recently been established in the private sector such as the AMR Action Fund. The Fund, set up by 20 leading pharmaceutical companies from the AMR Industry Alliance, is committed to investing $1 billion over the next few years in bringing two to four novel antibiotics to patients by 2030.
Yet, some experts argue that not enough action is being taken and call for a legally binding global treaty, similar to the Framework Convention on Tobacco Control as an overarching global mechanism to overcome the current piecemeal approach to combatting AMR.
Keeping the conversation going
From our end, the European Observatory on Health Systems and Policies has been working on this issue for many years, supporting countries in Europe by providing evidence on developing appropriate NAPs to ‘avert the AMR crisis’ and by supporting the development of governance tools to aid their implementation. We have also lent support to the EU Council Presidencies mentioned above in their efforts to advocate for more action. This year’s spring edition of Eurohealth is largely devoted to ‘Tackling antimicrobial resistance’. It was published as the deadly COVID-19 pandemic gripped the world, raising the issue of societal preparedness for such health crises and confronting critical issues that as yet do not figure as prominently as the coronavirus in public awareness.
COVID-19 has highlighted the fundamental importance of substantial investment in resilient health systems that can cope with and effectively respond to adverse shocks, such as pandemics. To that end, the Observatory will be supporting the works of the independent Pan-European Commission on Health and Sustainable Development: Rethinking policies in the light of the pandemic convened by the WHO Regional Office for Europe. The Commission will draw lessons from the national responses to the COVID-19 pandemic and make recommendations on investments and reforms to improve the resilience of health and social care systems.
AMR and pandemic preparedness will be among the key themes of this year’s annual European Health Forum Gastein (EHFG) conference, taking place in late September/early October, where the Observatory has been a longstanding participant and contributor. The first-ever virtual EHFG will bring together top European politicians, researchers, civil society activists, industry representatives, and journalists to discuss Europe’s most pressing health issues and stimulate action for radical change.
Keeping the conversation going in these unprecedented times amongst actors from government, industry, civil society and the public as a whole is essential for keeping AMR on the European and global radar while the coronavirus wreaks havoc across the globe and absorbs most of our attention. The COVID-19 pandemic has served immensely to raise the public understanding of infection prevention and control. The greater momentum behind this should, therefore, be leveraged to tackle AMR. It cannot be left as a pious hope but requires urgent action across the board. The AMR pandemic is predictable and can be prevented. We must not let it catch us off guard.
This article was kindly provided by the European Health Forum Gastein (EHFG).
This op-ed was written in early September hence any specific COVID-19 numerical references could be outdated at the time of publication.
The COVID-19 outbreak in the African Region
For further reading, you might like to look at Open Access Government’s interview with Dr Mary Stephen, Public Health Expert at the World Health Organization African Region. In the piece, Mary discusses in detail the ongoing COVID-19 outbreak since it was first reported in China back in December 2019. Certainly, we learn how governments and health authorities across Africa are striving to limit widespread infections. Ebola was a prominent infection issue in the region a few years ago, which the WHO was highly involved with in terms of understanding and containing it. Here, Mary outlines the transferable lessons WHO learnt from their work in this vein.
While manufacturers and scientists globally are estimating that a feasible vaccine will not arrive before 2021, a definitive timeline for this is still not easy to determine. Despite this, Mary stresses that COVID- 19 is real and highlights very strongly the importance of employing preventive measures like staying at home, hand washing, social distancing and cough etiquette. I’m sure you will agree that this important message still applies to us all, globally.
For daily updates on confirmed COVID-19 cases in the WHO African Region, please visit this link.
Please note: This is a commercial profile