63.8% of the UK population are currently overweight or obese. Obesity is a major cause of ill health. Being moderately obese takes around 3 years off your life, whereas severe obesity shortens it by at least 10 years.
Many people do not realise that being overweight or obese increases their risk of cancer. It’s a sad fact that obesity is now a bigger cause of cancer than smoking. This is particularly true for bowel, kidney, ovarian and liver cancers.
How does being obese cause cancer?
There are many physiological and biochemical reasons that obesity increases the risk of cancer. These are listed below –
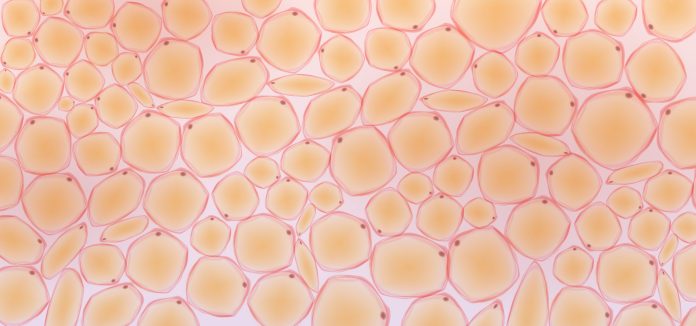
Fat is metabolically active
Fat is not inert. It is highly metabolically active and produces hormones such as hormones, cytokines and adipokines which increase the risk of cancer. Adipocytes (fat cells) produce estrogen, for example, which increases the risk of breast, endometrial and ovarian cancer as well as some other cancers.
Obesity and cancer: Increased insulin resistance
People who are obese often have abnormal glucose tolerance, leading to insulin resistance. This means the cells of the body have become resistant to insulin, and as a consequence, levels of insulin and insulin-like growth factor (IGF-1) are increased.
Insulin resistance is the first step in the development of type 2 diabetes (T2DM) which is itself a risk factor for cancer. 1 in 5 cancer patients have T2DM.
IGF-1 is known to inhibit apoptosis – the destruction of abnormal cells and stimulate cell growth. Raised levels of IGF-1 have been found in those with breast, bowel and prostate cancer.
High systemic inflammation
Obesity is linked to high levels of systemic inflammation. Studies have shown that obese people have higher levels of interleukin-6 (IL-6), a cytokine (a cell-signalling molecule) that activates the immune response.
IL-6 is produced by adipocytes. C-reactive protein (CRP) levels are also elevated. When the body is in a perpetual high inflammatory state as in obesity, these molecules stimulate cell proliferation (cell growth) and increase the risk of cell mutations (DNA damage that leads to cancer).
Changes in adipokines
In obesity, levels of the hormone leptin are increased. Leptin also increases cell proliferation. It works like a growth hormone, causing tumour cells to divide and multiply and encouraging new blood vessel formation. High leptin levels are strongly correlated with breast cancer, but they have also been linked to bowel, prostate, pancreatic, ovarian and lung cancers.
On the other hand, levels of the hormone adiponectin are lower in those with obesity. Adiponectin has anti-cancer effects, so anything that reduces the amount in the blood circulation increases cancer risk.
A range of other adipokines, such as apelin, visfatin and resistin, also play a role in cancer development.
Oxidative stress
Those with obesity often have other chronic diseases such as gallstones or fatty liver disease. These conditions increase oxidative stress. Every day each cell of the body is undergoing oxidation reactions to create energy for its cellular processes. As a byproduct of oxidation, negatively charged molecules are formed called reactive oxygen species (ROS). These are dangerous as they have the potential to damage DNA, and this probably underpins the development of many of the chronic diseases we see today, including cancer. Obesity is associated with increased oxidative stress.
Gut microbiome
Recent studies have shown a link between the microbiome and cancer risk. Obesity seems to change the microbiome in a way that promotes tumour growth. Evidence suggests that the microbiome of cancer patients who are obese contains large concentrations of specific gut bacteria. For example, Streptococcus bovis, Helicobacter pylori, Bacteroides fragilis, E. faecalis, Clostridium septicum, and Escherichia coli, are thought to play a role in the onset of bowel cancer.
Does losing weight lower the risk of cancer?
The good news is that losing a small amount, such as 5%—10% of your body weight, lowers your cancer risk.
In one 2017 prospective study, women who intentionally lost at least 5% of their body weight had a significant reduction in the risk of endometrial cancer in comparison to the group who maintained their weight. Moreover, those who gained weight in the study increased their risk of endometrial cancer.
In a 2023 review and meta-analysis of 32 studies looking at cancer risk in obese patients, those who had had bariatric surgery were found to have a statistically significant reduction in cancer and cancer-related deaths. These results were seen for cancers of the bowel, pancreas, breast, endometrium and ovary.
Final thoughts on the connections between obesity and cancer
There are clear mechanisms by which obesity causes cancer. We are unaware of these processes taking place in our bodies – which they do – all day, every day. The average cancer has been present for 10-20 years before diagnosis. What you do today will help your body not just now but well into the future.
- Is now the time to find a suitable weight loss program?
- How might you get started? What could you do?
For more information
- net – Body weight and cancer risk
- World Cancer Research Fund – Obesity, weight and cancer risk
- NHS – Obesity
This piece was written and provided by Dr Deborah Lee, Dr Fox Online Pharmacy