Estonia is leading in integrating genomic data into national healthcare, showcasing a model for personalised medicine as essential for sustainable healthcare, particularly for conditions like depression and breast cancer
Estonia is the first country in the world to integrate genomic data into everyday healthcare at scale, not as a pilot but as a national policy. Genetic screening for breast cancer and using DNA to guide medication prescription choices are already technically available for physicians and patients alike. But the real story isn’t just about medicine or algorithms. It’s about how Estonia made this possible through long-term investment in governance, digital infrastructure and public trust.
While other countries are still assessing if personalised medicine is scalable or ethical, Estonia is showing that with the right foundations, it’s already here.
Trust, not tech, is the foundation
Estonia’s genomic healthcare system did not begin with a technology purchase. It started with a commitment to public digital infrastructure more than 20 years ago, when national ID, interoperable records and a secure data exchange layer (X-Road) were still radical concepts.
These elements laid the groundwork for something many governments still struggle with: public trust in data-driven services. Today, a significant portion of Estonians have voluntarily contributed their genetic data to the national biobank, managed by the Estonian Genome Centre. This opt-in participation is embedded in the patient experience, from the national portal to clinical workflows.
Why do people take part? The benefits are tangible: tailored treatment, early detection, and the ability to manage their health data. People aren’t just giving data away. They’re getting something meaningful in return.
Don’t regulate the tech. Regulate the model
Estonia didn’t just build a platform. It redesigned how genetic data flows through the public healthcare system.
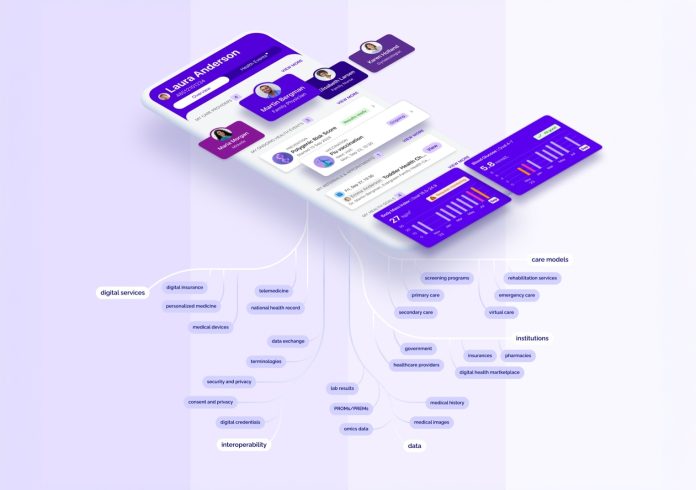
Here’s how it works: algorithms to assess genetic risk or guide prescriptions are hosted in a secure national computation environment. These algorithms pull from the national health record and biobank data and feed their results directly into clinical documentation. Physicians see those results in their normal workflow. Patients see them in the national portal.
Importantly, the platform tracks which algorithms are used, when and how. It manages consent, triggers new calculations when required, and ensures auditability, not just for compliance but to support innovation and product improvement. Crucially, patients have full control over which algorithms are used and when through an opt-in system that respects individual preferences.
This model of algorithmic governance is what makes the system scalable and safe. Estonia has shown that technology doesn’t need to be perfect from the start; it needs to be governable from the start.
Personalised medicine as a system fix, not a luxury
While much of the global discourse focuses on the science of genomics, Estonia frames personalised medicine as a tool for system sustainability.
Take depression. It’s one of the most costly and complex health burdens worldwide. Traditional prescribing is often trial-and-error, leading to delayed recovery, side effects, and waste. Estonia’s pharmacogenomic service supports doctors in prescribing more effectively from the start, a shift that could save tens of thousands of euros per patient over time.
Or breast cancer. Women can now order genetic testing directly via the national portal. If high risk is identified, they’re added to screening programs earlier, increasing the odds of early detection and survival. That’s not just better care; it’s smarter use of resources.
Personalised medicine helps shift healthcare from reactive to preventative and from average-based to individualised. That’s where the long-term savings and system resilience lie.
Four lessons for policymakers
Estonia’s progress wasn’t inevitable. It came from decisions, some of them made decades ago. For governments interested in following suit, here are four principles that made the difference:
Invest early in digital foundations
National ID, interoperable records and secure data exchange aren’t glamorous. But without them, personalised medicine at scale is unworkable.
Design for citizen control
Opt-in participation and clear, accessible consent management build the trust that data-driven services rely on. Estonia’s patient portal puts people in charge of their own genetic data.
Embed innovation into existing services
Estonia didn’t create new standalone systems. It upgraded public healthcare with genetic functionality. Doctors use the same tools. Patients follow the same paths.
Govern the service, not just the technology
What matters is not just the algorithm but how it’s triggered, audited and integrated. Estonia built a model that supports transparency, continuous improvement, and safety.
From promising science to public service
This is not a story about a successful tech project. It’s a story about governance. By aligning infrastructure, consent, regulation and service delivery, Estonia has turned the idea of personalised medicine into a routine public service. Other governments can follow, not by copying the tech stack, but by adapting the principles: build trust, design for scale and treat digital health innovation as a matter of long-term policy, not short-term projects.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.