Emily Y. Chew, M.D., Director of the Division of Epidemiology and Clinical Applications and the Deputy Clinical Director at the National Eye Institute, part of the National Institutes of Health, examines why early detection is crucial to prevent blindness from diabetic retinopathy
Regularly getting an eye exam is a key action people with diabetes can take to safeguard their vision. Diabetes not only doubles one’s risk for cataracts and glaucoma, but it can lead to diabetic retinopathy. According to the Centers for Disease Control and Prevention, diabetic retinopathy is among the leading causes of blindness and low vision in the United States.
Biomedical research
Biomedical research has produced remarkable advances in our ability to treat diabetic retinopathy. First, laser photocoagulation in the 1980s and 1990s was able to slow serious vision loss. Then, in 2010, clinical trials demonstrated that injections of anti-vascular endothelial growth factor (VEGF) could reduce vision impairment from diabetic macular edema, a subtype of diabetic retinopathy and the leading cause of vision impairment from the disease.
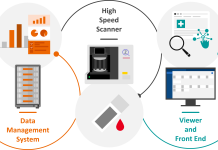
Concurrently, bioengineers developed imaging technologies, such as optical coherence tomography, which measures swelling of the light-sensitive retinal tissue at the back of the eye. The ability to image the retina in such detail has radically improved our ability to follow patients over time, so we can adjust treatment strategies as needed.
Yet, despite these diagnostic and therapeutic leaps forward, our ability to optimally leverage these advances depends on patients and eye health professionals detecting the disease in its early stages.
Eye exams
About one in three people with diabetes have diabetic retinopathy but are unaware he or she has it because, in its early stages, it is symptom-free. The best way for a patient or eye health professional to identify diabetic retinopathy is through a comprehensive dilated eye exam, which allows viewing of the retina at the back of the eye.
Timely eye exams are necessary to take advantage of the available treatments. The American Diabetes Association advises people with Type 2 diabetes to receive an eye exam as soon as possible after their diabetes is diagnosed. Those with Type 1 diabetes should have the exam within five years of diagnosis. The schedule for regular follow-up exams thereafter is every one or two years depending on the patient’s risk.
Diabetes leads to complications, such as heart, kidney and eye disease by affecting large and small blood vessels in the body. In the case of late-stage retinopathy, new small vessels grow abnormally in the eye. The fragility of these vessels makes them prone to rupture, which can cause bleeding inside the eye and potentially detachment of the retina, leading to blindness.
At any stage of retinopathy, inflammation and other factors cause the accumulation of fluid or edema, within the retina. When a person develops macular edema – occurring in the area of the retina that enables sharp, central vision – it results in the loss of vision required for activities such as reading or seeing faces.
Risks
The risk of developing retinopathy increases the longer a person has diabetes.1 It is estimated that individuals with Type 2 diabetes have a 50-60% lifetime risk of developing retinopathy, while those with Type 1 diabetes have up to a 90% lifetime risk. Of those who develop the disease, 5-10% of them progress to late-stage disease.
Much progress has been made in understanding the underlying pathology that leads to diabetic retinopathy. High blood glucose levels can lead to degeneration of neurons in the retina. At the same time, high blood glucose levels are associated with abnormalities of small vessels in the eye and to the neurovascular unit, a complex unit of cells that regulates blood flow to neurons.
These insights about pathology inform the steps that patients are advised to take to limit their risk as much as possible. The good news is that several studies demonstrate that the risk of developing retinopathy or having it progress to later stages is lowered significantly when diabetic patients tightly manage their blood glucose and blood pressure levels. Achieving optimal blood glucose and blood pressure targets require adhering to drug therapy and a healthy lifestyle, including diet, exercise and smoking cessation.
Lack of lipid control also contributes to diabetic retinopathy. Some studies have demonstrated that persons who have better control of their dyslipidemia have less diabetic retinopathy progression.
A look at the future
Finally, although advances such as laser coagulation and anti-VEGF therapies have been a game-changer for managing diabetic retinopathy, they are not a cure.
Researchers including those funded by the National Eye Institute continue to explore other potential therapeutic targets for preserving vision on behalf of the growing population of people who develop diabetes. According to the CDC, the number of Americans with diabetic retinopathy is expected to grow to 14.6 million by 2050.
In addition to having a comprehensive dilated eye exam, following these simple steps can help everyone stay on top of their eye health.
References
1 Klein, R., Klein, B. E., Moss, S. E., Davis, M. D. & DeMets, D. L. The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch. Ophthalmol. 102 (1984).