Here, the tangible impact on diabetes patients and their care is thoroughly explored via integrated personalised diabetes management (iPDM)
Treatment inertia calls for an integrated personalised diabetes management: iPDM.
Despite the availability of numerous treatment options, many patients still fail to reach their treatment goals. According to the UK National Diabetes Audit data 2016-2017, only 30% of people with Type 1 diabetes and 67% of people with Type 2 diabetes achieved a HbA1c target of not more than 58 mmol/l (7.5%). This is all the more remarkable as diabetes represents a huge challenge for European societies.
The good news for innovators tackling treatment inertia in people with Type 2 diabetes, is that this disease leaves a huge space for advancing diabetes treatment towards an iPDM. Personalisation is considered key for overcoming treatment inertia and narrowing the well-known discrepancy between drug efficacy, found in well-controlled clinical trials and drug effectiveness, observed in real-world clinical practice (the E2E gap).
iPDM: the conceptual roots
In 2012, Antonio Ceriello and colleagues published a concept paper proposing a structured and iterative six-step process cycle for the implementation of a prototypic iPDM regime:1
- Education & training for a structured self-monitoring of blood glucose (SMBG)
- Implementation of structured SMBG
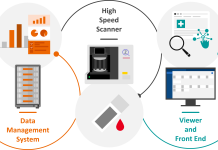
- Upload and documentation of SMBG data
- SMBG data analysis
- SMBG data-based adaption of treatment
- Assessment of treatment efficacy
Repeatedly entering new cycles of iPDM was proposed to realise an iterative approach, enabling a stepwise optimisation of the individual diabetes management.
iPDM-like cycles in diabetes management were taken up in a recent consensus report on the management of hyperglycemia in Type 2 diabetes of the American Diabetes Association and the European Association for the Study of Diabetes.2
Real-World effectiveness of iPDM: the ProValue study program
Inspired by the iPDM proposal, the iPDM-ProValue real-world studies were initiated.3 iPDM-ProValue integrated low-threshold digital tools to prove the effectiveness of a 12-month iPDM regime in people with Type 2 diabetes on insulin therapy. They were designed as prospective, cluster-randomised, controlled intervention trials comparing iPDM in either general medical or diabetes specialised practices to a control group.
Overall the iPDM-ProValue studies indicated that patients following the iPDM scheme achieved better glycemic outcomes. The better reduction of HbA1c after 12 months iPDM vs. usual care (- 0.5%, p < 0.0001 vs. – 0.3%, p < 0.0001; Diff. 0.2%, p = 0.0324) was achieved without any impact on the incidence rate ratio of hypoglycemic episodes. At the same time in the iPDM groups a higher percentage of patients received recommendations to adjust their insulin therapy and experienced more behavioural and lifestyle recommendations throughout the study. Also, the satisfaction of both patients and healthcare providers as well as the adherence of patients to their pre-determined treatment regimens improved in the iPDM groups. iPDM effectiveness was positively affected by the usage of digital tools.
iPDM-GO: from real-world validation studies towards Europe-wide implementation
The recently started iPDM-GO (iPDM Goes Europe) initiative involves a consortium of diverse partners from industry, academia and healthcare administration in Europe. Collectively, the team has extensive expertise and skills in clinical practice, computer science, health psychology, health economics and bioinformatics. Profil is coordinating a workpackage on “Research in iPDM enhancement, implementation and scalability” and adds expertise in close-to-market clinical research and development.4
iPDM-GO takes advantage from the dedicated innovation eco-system provided by the European EIT Health public-private partnership.5 This is going to facilitate the engagement with all the involved stakeholders which is essential for a successful launch of iPDM. iPDM-GO is dedicated to implementing iPDM, along with an outcomes-based payment model, first in innovative model regions to lay groundwork for expanding these concepts to additional European countries.
iPDM enhancement: for tangible impact on diabetes patients and diabetes care
The iPDM-GO initiative realises an open and collaborative approach. It is answering the challenge of how many people with diabetes still do not achieve their treatment goals – while the costs associated with chronic diseases continue to rise.
iPDM-GO offers opportunities to further enhance iPDM and explore the massive and multi-dimensional scalability of iPDM. Acknowledging the diversity of people with Type 2 diabetes is key for the implementation of iPDM regimens people are able and willing to adhere to. Health economic analysis needs to be applied in order to prove the cost-effectiveness of iPDM evolution.
Patient assessment should integrate the usage of real-world data collected by sensors combined with telemedical tools. Applying machine learning approaches to large epidemiological data sets will help to establish prediction models estimating the individual risk of developing comorbid conditions. Integrating advanced artificial pancreas systems as developed by the CLOSE EIT Health innovation project6 for a comprehensive monitoring of health and disease signatures will produce a huge amount of real-world data informing iPDM by taking advantage of self-learning control algorithms. Data-driven iPDM feedback loops will trigger an adjustment of therapies, social interventions and behavioural patterns along the lines of patient preferences, new drugs & technologies, treatment guidelines, geography and reimbursement policies, to name a few – leading to an amelioration of treatment inertia and the E2E gap with a tangible impact on the life of diabetes patients and the sustainability of diabetes care.7
References
1 Ceriello, A. et al., Diabetes Res. Clin. Pract. 98(1):5-10, 2016
2 Davies, M. et al., Diabetes Care 41(12):2669-2701, 2018
3 Kulzer, B. et al., J. Diabetes Sci. Technol. 10(3):772-780; Kulzer, B. et al., Diabetes Res. Clin. Pract. 144:200-212, 2018; Heinemann, L. et al., J. Diabetes Sci. Technol., doi: 10.1177/ 1932296819867686. [Epub ahead of print], 2019
4 https://www.eithealth.eu/en_US/ipdm-go
6 https://www.eithealth.eu/en_US/close
7 Schliess, F., https://www.eithealth.eu/digital-diabetes, 2019
The iPDM-GO and CLOSE innovation project is supported by EIT Health, a network of best-inclass health innovators that collaborates across borders and delivers solutions to enable European citizens to live longer, healthier lives. EIT Health is supported by the EIT, a body of the European Union.
Please note: This is a commercial profile