PillTime Ltd highlights the importance of medication management for diabetes as it remains a significant burden on the NHS
As we look to the future of the NHS, diabetes remains a significant burden. Estimates show that as many as five million people in the UK will have diabetes by 2025.1 By any standards, this is a huge diabetic population.
Every year, the NHS spends at least £10 billion on treating diabetes. That’s an unfathomable £1 million every hour.2 The financial implication of diabetes to the NHS is great. Yet, it’s not the cost of treating the illness itself that is so encumbering. The complications that arise from poorly-managed diabetes are vast and costly. A 2012 report from the London School of Economics sheds light on the issue. It estimates that diabetes complications cost around three to four times more than the cost of prescribing diabetes medication.3
Diabetes complications include blindness, amputation, heart disease and stroke. These outcomes can be devastating to sufferers and family members. They also place undue pressure on the NHS.
The bitter pill to swallow? These dangerous and expensive complications are, most often, entirely preventable
People with diabetes can control their condition by taking good care of themselves. This includes eating a healthy diet, being active and taking the correct medication. These are all ways to maintain safe and stable blood sugar levels. This, in turn, reduces the risk of extensive health issues. Diabetic people can live long and healthy lives with the illness.
In spite of this, medication adherence amongst Type 2 diabetics (T2D), in particular, is low. More than 500 people with diabetes die prematurely every week. On average, one in six hospital beds is occupied by someone with diabetes.2
Why is medication management so poor and how can we improve it?
People with diabetes often have several medications to manage their symptoms, as well as their blood sugar. Plus, T2D often arises from a poor lifestyle and obesity. Because of this, people with T2D may likely be managing other associated health issues. Common troubles include high cholesterol, high blood pressure and issues around mental health. This can add an extra layer of daily medication on top of an already hefty diabetes treatment plan.
When taking an array of different prescription drugs, it’s easy to get things wrong. People often miss doses or take the wrong thing altogether. Organising many medications can be confusing and time-consuming. As an experienced pharmacist, I’ve known many patients who struggle to manage their doses. I’ve even seen medication wrapped in stray bits of tinfoil, unlabelled, used as a dose solution. Dose-sorting needs to be rigorous and thoroughly checked. Patients are not always able to do this for themselves.
Medication non-adherence: The risks
For decades, healthcare professionals have been aware of these issues. Poor medication adherence isn’t exclusive to people with diabetes. In fact, more than 50% of people take their medication incorrectly. This figure increases with age and the number of items a person takes.4 If people don’t take their medication as instructed by their doctor, they do not get the full benefit of it. They may also be putting their health at risk.
Poor medication management can have severe consequences. These include withdrawal symptoms, poor condition control and hefty NHS costs. Wasted medication alone costs the NHS over £300 million every year.5 That’s before the cost of hospital and GP resources needed to treat people who are suffering as the result of poor medication management. The NHS can’t sustain these avoidable burdens. As we take on the NHS’s Long-Term Plan, it’s imperative that we tackle adherence in a holistic way.
The limitations of compliance aids for diabetes medication
Traditional compliance aids, such as dosette boxes, are used to help tackle to problem. However, these aids can often present further challenges. Medication is personal; everyone’s needs, lifestyles and struggles are different. Dosette boxes don’t account for this and may result in people incorrectly amending their doses to fit into rigid dosing times. Plus, not everyone wants to lug their whole week’s worth of medication around. It’s inconvenient to crack open a medication tray at a business meeting, a coffee date or the gym. This can deter people from taking their dose when they need it.
PillTime has revolutionised medication management
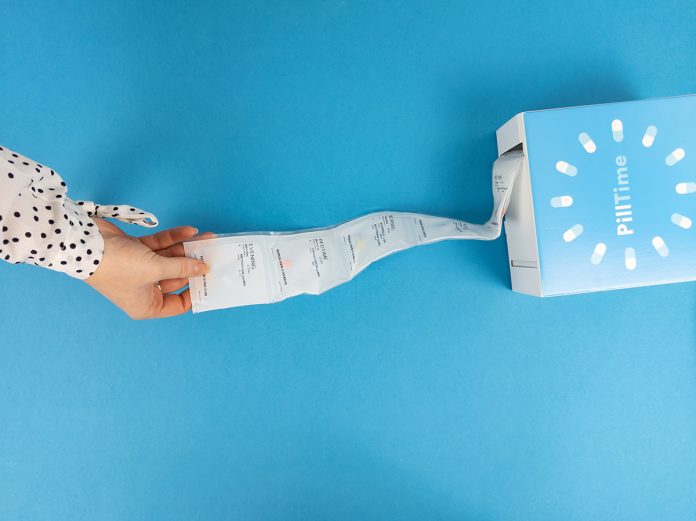
Now there’s a free solution that revolutionises medication management, once and for all. We created PillTime digital NHS pharmacy in 2016. Ever since, we have been helping thousands of people manage their prescription. We dispense everything needed for one dose into a clearly-labelled, easy open pouch. The whole prescription is organised onto a reel of pouches, in the order they need to be taken. So, patients simply tear off their required pouch, and the rest stays organised in their PillTime box. We use robotic technology and image recognition to sort and check the pouches as part of a rigorous checking process.
How does PillTime help improve diabetes medication management?
It removes the hassle and confusion. We organise everything for our patients. So, there’s no need to worry about sorting doses and working out the best time to take it. We take personal needs into account and clearly label each dose with a person’s name, their time of dose and a full description of the contents. This way, it’s plain to see what’s required and when. In addition, medication management is no longer restrictive. Our pouches can be taken on the go, so there’s no compromise between lifestyle and health.
PillTime’s personalised solution is ideal for people with diabetes. As well as the pouches, we deliver all prescription items in one free delivery. A PillTime delivery contains all non-tablet medication, such as injections and testing strips. By making prescriptions hassle-free, convenient and personalised, we remove everyday obstacles that arise for people taking several medications. Our pouches fit seamlessly into people’s routines. When medication simply becomes part of someone’s day, they are more likely to take it properly. This in turn, aids condition management and reduces the need to seek medical help.
PillTime makes managing multiple medications simple. To find out more about our free service, or to enquire about working with us to help improve adherence and reduce NHS costs, visit our website, at www.pilltime.co.uk .
References:
1 https://www.diabetes.co.uk/diabetes-prevalence.html
3 https://www.diabetes.co.uk/cost-of-diabetes.html
4 World Health Organisation. (2003). The World Health Report 2003: Shaping the Future. http://www.who.int/whr/2003/en/whr03_en.pdf Accessed 21.08.18.
5 NICE. (2015). Medicines optimisation: the safe and effective use of medicines to enable the best possible outcomes. https://www.nice.org.uk/guidance/ng5/chapter/1-Recommendations Accessed 21.08.18.
Please note: This is a commercial profile
Hannah Matthews
Marketing Executive
PillTime Ltd.