Andrea Ammon, Director at the European Centre for Disease Prevention and Control, takes us on a journey from COVID-19 to the future of public health surveillance
When the European Centre for Disease Prevention and Control (ECDC) was founded in the aftermath of the SARS epidemic 15 years ago, it set out to provide standardised and comparable infectious disease data across the EU. We did so by establishing the European Surveillance System, TESSy – a technical platform for web-based data collection. Since then we have worked hard, together with the Member States, to establish standardised reporting and data comparability across the EU.
Pandemics and public health surveillance
However, since the early days of the COVID-19 pandemic, many EU Member States encountered difficulties in establishing robust, population-based surveillance systems to deliver reliable and timely data on COVID-19. Countries have also struggled to maintain a high testing and contact-tracing capacity. And despite considerable efforts, collaboration and dedicated work of many colleagues in the Member States and at ECDC, we are experiencing the challenges of providing data that are comparable across a range of indicators for the EU and EEA countries. Some of the reasons lie in electronic systems, from where most data originate, not being designed to inform surveillance.
To prepare for future pandemics, health systems should be able to accurately capture valid data on population health on an ongoing basis, covering large populations. If comprehensive syndromic surveillance for acute respiratory infections (ARI) and severe acute respiratory infections (SARI) were in place, it would have detected the start of the COVID-19 pandemic in the EU much earlier than border controls and targeted testing did. This would have also allowed for better monitoring of the epidemic when the true number of cases was hidden by limited testing capacity. Furthermore, data systems interoperability should be raised to a new level, driven by a public health purpose and encompassing metadata information in order to enable in-depth, unbiased analyses of incidence, severity, risk factors and sequelae of COVID-19 and other diseases.
Innovative technological solutions
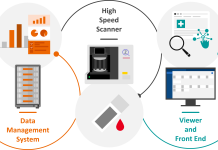
We also need to look into innovative technological solutions such as digitalised electronic reporting or artificial intelligence (AI) in order to decrease workloads and increase timeliness. And we need to consider building up surveillance systems where human input is needed at the design and interpretation stage, but that the system is otherwise mostly automatic. To achieve this, significant changes are needed, including comprehensive electronic health records coverage and standardisation of information collected. Furthermore, scrupulous validation studies are needed before information from such records can be used for public health action.
In Europe, most countries have started with the digitalisation of healthcare, among others with electronic health records, electronic prescriptions that can be shared across borders, electronic immunisation information registries and now during the pandemic, contact tracing apps.
However, many issues still remain to be solved such as:
- How we transition from burdensome notification systems to digital epidemiology?
- How we capture data at its source and enable instantaneous and seamless application of data for decisions and strategies in disease prevention and control?
- How we ensure transparency so that individuals know what happens to their health data, have access to their health data and are involved in how and what for these data are used?
- How we ensure the safety and protection of the data?
- And finally, how we make the technologies interoperable across borders?
The ongoing pandemic, and our response to it, has been the biggest test to all our systems, resources and policies that we have ever experienced in our lifetime. On a daily basis, it has required urgent action at the national, European and global level, often stretching us to the limits of our current capacity.
ECDC’s objective is to close existing knowledge gaps, to reduce inequities between the countries and help find solutions for legal, ethical and privacy concerns. Not of least importance – we must ensure that the needs of key public health functions are taken into account when developing eHealth and digital health strategies and implementation plans on national and EU level. ECDC sees it as its task to support the Member States in making the transition to adopt new technologies for improving public health.
The future of public health surveillance
At ECDC, we consider that the further digitalisation of health information will ultimately result in more data of better quality with less effort for experts involved in infectious disease surveillance. One of our current priorities is to assess and integrate innovative technological and scientific advances to routine work and in particular, the use of whole-genome sequencing, e-health, big data, and social media for surveillance.
On 11 November 2020, the European Commission presented a set of proposals to the Council and the European Parliament aimed at expanding the legal mandate of ECDC. Epidemiological surveillance via integrated systems enabling real-time surveillance is one of the proposed changes whereby the Centre may support the Member States and the Commission.
In parallel, a proposal for a new Regulation on serious cross-border health threats was announced aiming to reinforce surveillance by creating a strengthened, integrated surveillance system at EU level, using artificial intelligence and other advanced technological means. Furthermore, to improve data reporting, Member States will be required to step up their reporting of health systems indicators.
We should use this pandemic to learn how to further improve our surveillance systems and build capacity and resilience in the public health systems in order to be better prepared for the next crisis. Unlocking the potential of data and of further digitalisation can result in patient empowerment, increased efficiency and cost-savings in health care.
This article follows Andrea Ammon’s participation in the European Health Forum Gastein (EHFG) online event during October 2020.