The ultimate goal of preventive cardiology should be to eliminate cardiovascular morbid events as a cause of death and disability
This strategy takes on greatest importance in societies in which life expectancy has already been prolonged by control of other preventable factors driving premature deaths.
The tradition in clinical and public health practice has been to identify and modify risk factors, which have been established over the last half century as modifiable predictors of cardiovascular morbid events. The most widely accepted predictors have been elevated resting blood pressure, increased body mass index and elevated low-density lipoprotein levels in blood. Efforts at controlling blood pressure, reducing body weight and lowering cholesterol levels have therefore been at the core of preventive cardiology.
Guidelines for medical management have advocated diet and exercise to reduce risk factors and targeted drug therapy to control elevated levels of blood pressure and cholesterol when these targets are at levels statistically associated with an increased risk of morbid events. This strategy has not resulted in most at-risk patients receiving effective preventive dug therapy (1), nor has diet and exercise reduced the risk of morbid events (2).
The benefits of diet and exercise
In the most ambitious effort to document the benefit of diet and exercise, a group of National Institute of Health-funded investigators undertook what they hoped would be a definitive documentation of the benefits of diet and exercise in a trial called Look Ahead, the results of which were published more than 8 years ago in the New England Journal of Medicine (2).
More than 5,000 overweight, diabetic men were randomly assigned to be returned to their health care provider for usual care or to be assigned to an aggressive program in supervised exercise and dietary management. Compliance with the management was remarkably high and the usual risk factors were favourably affected. But after nearly a decade of follow-up, cardiovascular morbid events exhibited no significant reduction or even a trend for a benefit in the treated group.
This negative trial could have influenced the medical community to question the current management strategy, but it instead has largely resulted in dismissal of the study as “flawed”. The medical community is so invested in the current management strategy that they hesitate to question the benefits of diet and exercise.
The medical community and the public have been trained to view elevated cholesterol and high blood pressure as the disease that needs treatment. But the disease is in the blood vessels and the heart. It is a progressive biological process that ultimately affects the ability of the coronary, cerebral, lower extremity, and renal arteries to deliver adequate nutrition to the organs. In the heart a structural process of myocardial cell growth and remodelling may be initiated and progress to left ventricular chamber enlargement and reduced pumping capacity. These biological processes in the arteries and heart represent the disease, not the risk factors that we are accustomed to targeting. Diet and exercise may modify the risk factors but do not necessarily slow the disease process. Appropriate drug therapy appears to treat the disease.
Non-invasive methods
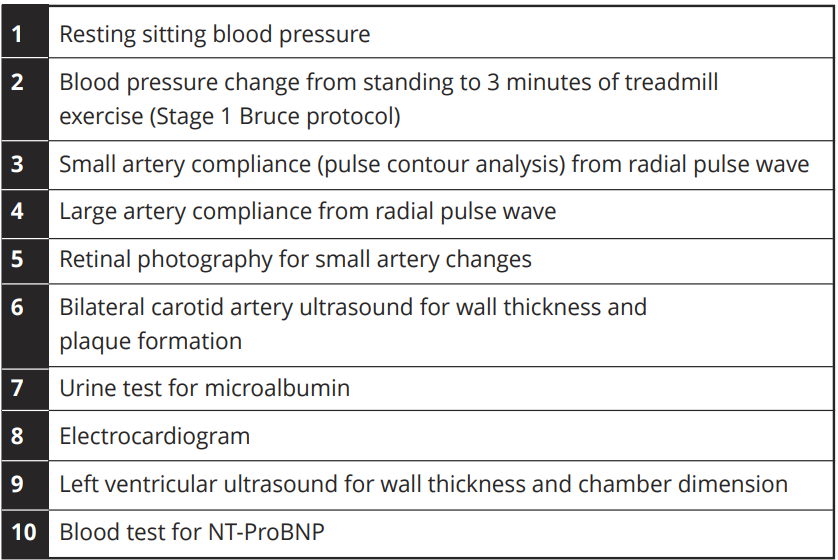
Fortunately, the health of the arteries and heart can be assessed by non-invasive methods that can easily be performed in a clinic environment (Table 1) (3). Each test is scored 0 for normal, 1 for borderline abnormal and 2 for abnormal. Some are corrected for age. A total score of 0-2 is defined as normal, a score of 3-5 as early disease and a score of 6 or greater as advanced disease. Follow-up of our patient population has demonstrated a striking effect of disease score on an individual’s risk for a future morbid event (4).
The ability of these simple procedures to quantify early disease severity, in the absence of symptoms, provides an opportunity to identify the characteristics and severity of early disease and therefore determine who needs treatment with what intervention to slow disease progression to morbid events. The difficult challenge of documenting that a given therapy can reduce future morbid events in asymptomatic adults can therefore be transformed into a process to slow asymptomatic disease progression, thus confirming that the intervention should prolong healthy life expectancy (5,6).
The 10 tests identified in Table 1 require specialised equipment and technical expertise that may not be readily available in clinical environments. We have therefore explored the potential of a simplified screening utilising the first four tests identified in Table 1. These can be performed in about 15 minutes in a clinic without expensive instrumentation or technical expertise. A positive screening result, suggesting the presence of early disease, can then serve as a guide to who needs additional study or treatment and who can be reassured of their cardiovascular health. The cost-effectiveness of this approach to prevention needs further study but has the potential of a shift in strategy from efforts aimed at morbid event prevention to the more assessable effort at slowing progression of cardiovascular disease. Application of the full 10-test evaluation could then be confined to populations in which more precise individualized care can be justified.
The cost of the screening and evaluation will always be an important consideration. If premature cardiovascular disease is a significant contributor to death and disability in any society, then efforts to identify those at risk and to institute effective therapy should be justified.
References
- Miedema MD, Cohn JN, Garberich RF, Knickelbine T, Graham KJ, Henry TD. Underuse of cardiovascular preventive pharmacotherapy in patients presenting with ST-elevation myocardial infarction. Am Heart J 2012;164:259-267.
- The Look AHEAD Research Group. Cardiovascular effects of intensive lifestyle intervention in Type 2 diabetes. N Engl J Med 2013;369:145-54.
- Cohn JN, Hoke L, Whitwam W, Sommers PA, Taylor AL, Duprez D, Roessler R, Florea N. Screening for early detection of cardiovascular disease in asymptomatic individuals. Am Heart J 2003;146:679-685.
- Duprez DA, Duval S, Hoke L, Florea N, Grandits G, Carlson C, Lee J, Cohn JN. Early cardiovascular structural and functional abnormalities as a guide to future morbid events. Eur J Prev Cardiol 2020 Feb 4:2047487320901416. doi: 10.1177/2047487320901416. Online ahead of print. Eur J Prev Cardiol. 2020. PMID: 32019367
- Duprez DA, Florea N, Jones K, Cohn JN. Beneficial effects of valsartan in asymptomatic individuals with vascular or cardiac abnormalities. J Am Coll Cardiol 2007;50;835-839.
- Cohn JN. Cardiovascular disease progression: a target for therapy? Am J Med 2018;131:1170-1173.
*Please note: This is a commercial profile
© 2019. This work is licensed under a CC BY 4.0 license.











