A universal receptor system that enables T cells to recognize any cell surface target has been created, to revolutionise customizable immunotherapies for treating cancer
Enabling highly customizable CAR T cells and immunotherapies for treating cancer and other diseases, the research has the potential to extend into solid tumors. This development would give more patients access to the life-changing results CAR T cell therapy has produced in a number of blood cancers.
SNAPtag: Enabling customizable immunotherapies and CAR T cells
The new approach involves engineering T cells with receptors bearing a universal “SNAPtag” that fuses with antibodies targeting different proteins. By tweaking the type or dose of these antibodies, treatments could be tailored for optimal immune responses.
“engineering T cells with receptors bearing a universal “SNAPtag” that fuses with antibodies targeting different proteins”
The SNAP approach was proven to work in 2 important receptors:
- CAR receptors, a synthetic T cell receptor that coordinates a suite of immune responses
- SynNotch, a synthetic receptor that can be programmed to activate just about any gene.
With SNAP showing its potential, the possibilities for customized therapies grow exponentially.
Creating a universal SynNotch receptor
“We showed for the first time that we can make a universal SynNotch receptor. This SNAP-SynNotch system is super programmable because you can have both designer input and designer gene output,” said senior author Jason Lohmueller, Ph.D., assistant professor of surgery and immunology in the division of surgical oncology at the Pitt School of Medicine and investigator at UPMC Hillman Cancer Center.
“Our hope is that we can use this approach to make cell therapies and deliver genes for cancer, autoimmune disorders, organ transplantation tolerance and more.”
“Our hope is that we can use this approach to make cell therapies and deliver genes for cancer, autoimmune disorders, organ transplantation tolerance and more.”
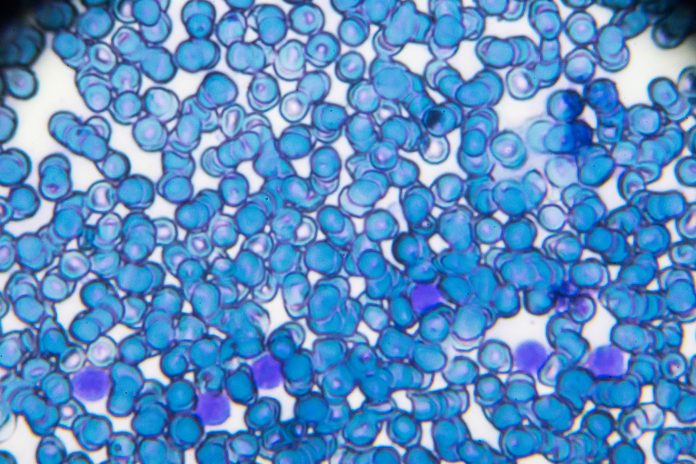
CAR T cell immunotherapy
“One of the big problems with CAR T therapy is that you’re targeting just one protein,” explained Lohmueller. “If the tumor evolves to lose that protein or downregulate it, you need to re-engineer the T cells a second time, which is a highly involved and expensive process.”
CAR T cell immunotherapy involves engineering a patient’s own cells so that the T cell receptor recognizes a specific protein on cancer cells before infusing them back into the patient.
Following these difficulties, a collection of the team were able to develop universal SNAP-CAR T cells by adding a SNAPtag enzyme to the CAR receptor.
According to the research published in Nature Communications, adding different antibodies at the same time or one after another, allows the receptor to recognize different tumor features.
It’s not just binding, but fusing
“What’s unique about our approach is how the T cell interacts with the antibody. It’s not just binding, but fusing via covalent attachment — the strongest form of chemical bond,” explained Lohmueller.
“This type of bio-orthogonal approach has been shown to work in animals for imaging purposes, but we’re among the first to use it therapeutically, so we’re really pushing the boundaries of covalent technology.”
Creating a tighter bond to reduce antibody use
One advantage of this tight bond means that activation of the receptor can be achieved with lower doses of antibody, points out Lohmueller.
The covalent bond was also the secret ingredient for creating SNAP-SynNotch cells.
“When a SynNotch receptor is activated, mechanical pulling forces stretch the receptor to expose part of the protein, which is then cut to release a transcription factor that travels to the cell’s nucleus to turn on expression of a chosen gene”, explains the team.
“We found that we needed the strength of a covalent bond to tolerate that pulling force,” explained Lohmueller. “If we just had binding between receptor and antibody, the receptor would come apart and we wouldn’t get signalling.”
Avoiding cancer relapses and investigating customizable immunotherapies further
The researchers showed that their universal SNAP-CAR and SNAP-SynNotch receptors could be activated in response to different targets by adding the corresponding antibodies.
SNAP-CAR T cells were also able to simultaneously target multiple proteins on different types of cells, suggesting that they could help avoid cancer relapse due to variation in tumor targets or loss of those targets.