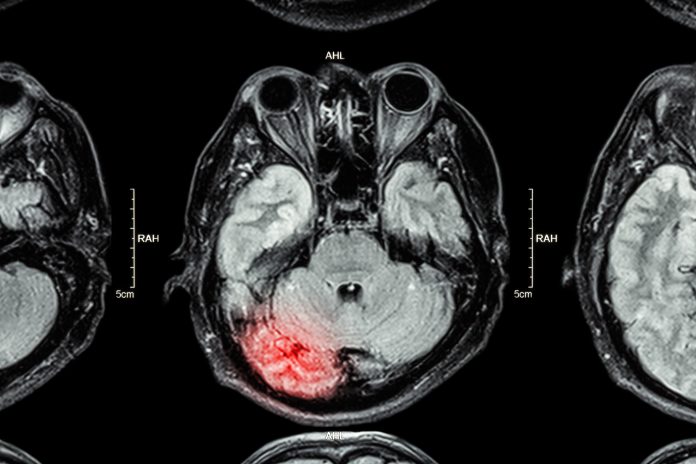
Ruth Smith, COO at Christchurch Group, applauds England’s 27 Major Trauma Centres provision of rehabilitation prescriptions for Acquired Brain Injury care
It’s a great step forward she says but why is it not mandatory and provided to all nationwide?
Hats off to MP Chris Bryant, Chair of the All Party Parliamentary Group on Acquired Brain Injury (ABI) for highlighting and continuing to lobby the Government regarding the poor state of the UK’s neurorehabilitation services since November 2017. Two years on I was delighted to hear that things have at last started to move with the introduction of a new directive to incentivise England’s 27 Major Trauma Centres to complete within 38-72 hours of admission a Rehabilitation Prescription (RP2019) that outlines the needs and care plan for patients when discharged.
It’s definitely a move in the right direction. For ABI patients whose lives have changed forever but are lucky enough to benefit from a neurorehabilitation care pathway it can mean the difference between returning home or a life spent stuck in a care home. But is it enough? What about those ABI patients who are located outside the catchment areas for these Centres – why shouldn’t they benefit from such opportunities, particularly as specialist rehabilitation is one of the most cost-efficient areas of healthcare provision in the NHS?
Earlier this year a report published by Neurological Alliance member charity Sue Ryder revealed that more than 15,000 people in England with complex neurological conditions such as head injury, motor neurone disease, MS, Parkinson’s disease and Huntington’s disease, are living in old people’s nursing homes.
This is shocking news and yet another case of the UK’s ‘postcode lottery’ in which access to health services and medical treatments is determined by the area of the country in which individuals live.
A strong body of evidence from around the world now demonstrates that early intensive rehabilitation following illness or injury is associated with better functional outcomes and earlier return to independence.
The British Society of Rehabilitation Medicine (BSRM) is a key collaborator. Findings published by them over the last decade show that even the most severely disabled patients make gains in independence through specialist rehabilitation that reduces their long-term care needs, providing substantial economic benefit to society.
According to the United Kingdom Acquired Brain Injury Forum (UKABIF) neurorehabilitation is one of the most cost-effective interventions available to the NHS. A report entitled ‘Specialist Rehabilitation following Major Injury (NCASRI)’ published in April this year found that in a group of 1381 individuals assessed as requiring specialist rehabilitation, only 40% received it. Those who did receive specialist rehabilitation did well, with 94% becoming more independent in their activities of daily living, which in turn reduced the costs of on-going care by an average of £536 per week.
Extrapolated over their lifetime, the average net life-time savings from neurorehabilitation amounted to just over £500,000 per patient, meaning that the total savings generated from this study group was £582 million.
Standards published by the BSRM recommend the early involvement of consultant specialists in rehabilitation medicine within the trauma and acute care pathways to ensure that rehabilitation is established as an integral care component within the major trauma centres and neuroscience networks.
What are we waiting for?