Romola Davenport and Richard Smith, Cambridge Group for the History of Population and Social Structure, Department of Geography, University of Cambridge explores the fascinating areas of cholera, water quality and public health in early Victorian cities
Before the twentieth century, it was almost always more dangerous to live in a city than in a rural area. A major cause of the risks associated with urban living was, and remains, gastrointestinal diseases, including cholera, dysentery, typhoid and other diarrhoeal diseases. These diseases are generally spread via ingestion of infected faeces in water and food or other sources of contamination, such as unwashed hands. Urban populations generate huge volumes of faecal waste, and this provides ample opportunities for gut pathogens to spread via contamination of wells and rivers, via flies or through inadequate domestic hygiene. The supply of clean water and the disposal of waste are, therefore, essential pre-requisites for healthy cities. Indeed readers of the British Medical Journal voted in 2007 for the ‘sanitary revolution’ (the introduction of clean water and water-based sewage disposal) as the ‘greatest medical breakthrough in history’. It is surprising, therefore, that historians have often struggled to demonstrate the obvious benefits of clean water and sewerage provision to the populations of Victorian cities.
Nineteenth-century British cities were at the forefront of developments in water supplies and sanitary engineering. The very rapid industrialisation of Britain in the late eighteenth and early nineteenth centuries was accompanied by unprecedented levels and rates of urban growth. Even London, already nearly a million in population by 1800 and the largest city in Europe, strained to cope with further growth in the early nineteenth century.
Contemporaries and historians have generally agreed, however, that it was the ‘new’ industrial and manufacturing towns that experienced the driest conditions and the highest mortality rates in this period as a consequence, in part, of rapid expansion and inadequate infrastructure. They also faced a new challenge in this period, in the form of lethal epidemics of ‘Asiatic’ cholera that repeatedly erupted in European and American cities between the 1830s and the 1890s. We might expect, therefore, that it was these newer towns, crowded with recent immigrants and jerry-built housing, that experienced the most serious cholera epidemics.
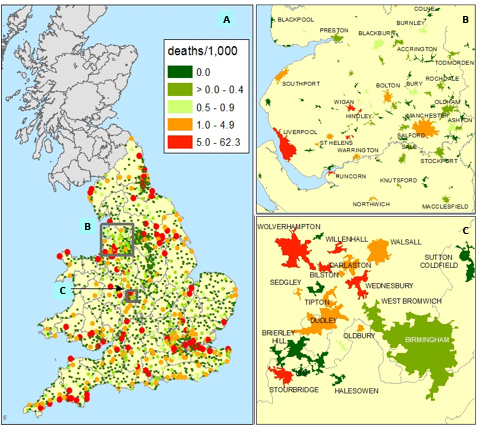
Surprisingly, however, while London suffered major outbreaks in all of the four cholera epidemics (in 1832, 1849, 1854 and 1866), many of the ‘new’ manufacturing and industrial towns of the Midlands and Northern England were only lightly touched by cholera. Figure 1 plots mortality rates from cholera for English and Welsh towns in 1849, before the waterborne nature of cholera transmission, had been demonstrated by John Snow.
In London, then a world leader in piped water and flush toilet technologies, cholera mortality was 5.9 deaths per thousand population. The port city of Liverpool experienced even higher mortality, of 11.3 deaths per thousand. However Manchester and many of the booming textile towns of Lancashire experienced relatively light mortality (panel B), and Birmingham escaped all four cholera epidemics virtually unscathed, despite its position as a major transport hub for canal and road transport, and its negligible provision of piped water (panel C). By contrast, the mining districts adjacent to Birmingham experienced some of the highest cholera death rates recorded.
What explains these unexpected geographical patterns of cholera mortality? Analyses of urban cholera mortality rates in 1849 demonstrate no association between the rate of growth of towns and their cholera mortality. Instead, they pick out the risk factors already identified by William Farr, the then Superintendent of Statistics: location on a major river, especially a tidal river or seaport, and mining districts. These were, in fact, the places with particular difficulties in supplying clean water to urban inhabitants as a consequence of their physical geography or peculiar development.
London was heavily reliant on its rivers, the Thames and the Lea, for water supply. The capital was precocious in the provision of piped water to its residents, supplying piped water to over 150,000 households, as well as street pumps, by 1828. This relatively copious provision of water-fuelled the adoption of flush toilets and this, in turn, led to the relaxing of a longstanding law against connecting household sewers to the public drains. The uncontrolled release of large quantities of sewage into London’s rivers resulted in widespread pollution of the city’s drinking water. When cholera was introduced by infected travellers, the contaminated river water was then piped efficiently into thousands of households. London had few alternatives to river water and, therefore, the improvement of the water supply required the construction of major sewerage and drainage works and the strict filtration of all river water (the abrogation of this rule caused the last great cholera outbreak in London, 1866).
Birmingham, by contrast, was slow to provide piped water but relied on large numbers of deep wells for most of its water supply. These wells were not easily contaminated by leakage from cesspits. Moreover, because they were numerous, contamination of a single well affected only the relatively small number of households that depended on that well, limiting the size of outbreaks. Manchester benefited similarly from the wide heterogeneity of water sources on which the population depended. Textile towns were particularly well-favoured because they were generally sited by fast-flowing and relatively clean streams on which they had originally depended for water power.
Mining towns, on the other hand, were often particularly deficient in water as a consequence of the lowering of the water table by mining operations, and the residents were often forced to depend on heavily contaminated water sources. Ironically, the backwardness of waste disposal could also be an asset for a town, since the use of cesspits and even midden heaps for waste disposal reduced the contamination of streams and rivers, compared with towns that had better sewers.
When Victorian towns did provide piped water, they often eschewed filtration in favour of unpolluted water from upland sources. By 1870, only three of England’s largest twenty cities had a filtered water supply, and these were all drawn from polluted river sources. In the 1850s, Manchester invested in a massive scheme to bring pure unfiltered water 50 miles from the Lake District to supply Manchester and Salford, the first long-distance supply scheme of its kind in Britain. This and other more local schemes have been under-rated by historians of public health, perhaps they lacked the precautions adopted so precociously but necessarily in London. Nonetheless, the sourcing of clean upland water in the 1850s and 1860s appears to have been sufficient to prevent waterborne transmission of cholera, typhoid and dysentery, well before the era of really major public investments in filtration and sewerage.
This research is supported by The Wellcome Trust, grant no. 103322/Z/13/Z, Migration, Mortality and Medicalization: The epidemiological consequences of urbanization 1600-1945
Please note: This is a commercial profile
Richard Smith
Emeritus Professor of Historical
Demography and Geography
University of Cambridge
Tel:+44 (0)1223 333 182
https://www.campop.geog.cam.ac.uk/research/projects/migrationmortalitymedicalisation/