Dr. Yuping Wang and Dr. David F. Lewis from LSUHSC-Shreveport discuss how to reduce hypertensive disorders in human pregnancy
The prevalence of vitamin D insufficiency/deficiency is a health problem worldwide, especially in pregnant women. Epidemiological studies revealed that about 40-60% of pregnant women are vitamin D deficient globally and the incidence of vitamin D deficiency can be as high as 90% of pregnant women in the developing countries [1].
Vitamin D insufficiency/deficiency in pregnant women
Many observational and meta-analytical studies demonstrated a strong relationship between low maternal vitamin D circulating levels in early pregnancy and increased incidence of pregnancy complications, including preeclampsia, preterm birth, infection rates, and gestational diabetes mellitus, which indicates that vitamin D deficiency is a risk factor for pregnancy complications and vitamin D supplementation is required for women during pregnancy.
Epidemiology of hypertensive disorders/preeclampsia
Hypertensive disorders in human pregnancy, including gestational hypertension, preeclampsia, and eclampsia, affect 2-8% of all pregnancies and are leading causes of maternal and fetal morbidity and mortality worldwide. Preeclampsia has been mostly studied in the past several decades. Based on data from the United States National Hospital Discharge Survey, the rate of preeclampsia in admission for labor and delivery increased by 25% from 1987 to 2004 [2, 3]. The rate was further increased as the data shown in the Health Cost and Utilisation Project (HCUP) statistical briefs, in which the total rate of preeclampsia/eclampsia among the delivery hospitalisations increased by 21% from 2005-2014 [4].
Data from the Health Care America Corporation revealed that preeclampsia was the second leading cause of pregnancy-related intensive care unit admissions after obstetric hemorrhage [5]. A systematic review by WHO showed that hypertensive disorders account for about 16% of all maternal deaths in developed countries, 9% in Africa and Asia, and as high as 26% in Latin America and the Caribbean [6].
Report also indicated that approximately 12 to 25% of fetal growth restriction and small for gestational age infants as well as 15 to 20% of all preterm births are attributable to preeclampsia [2]. Furthermore, emerging evidence also points out that preeclampsia is not only a risk factor for cardiovascular diseases in women later in life, but also a risk factor for long-term cardiovascular morbidity of the offspring later in life [7]. Therefore, prevention and reduction of the incidence and severity of hypertensive disorders in human pregnancy is a global health issue for both the mother’s own well-being and the healthy development of the baby during pregnancy and their children later in life.
Non-bone function of vitamin D
Vitamin D is a group of fat-soluble secosteroids. In humans, vitamin D2 (25(OH)D) and vitamin D3 (1,25(OH)2D) are the two most important compounds in this group. For a long time, vitamin D has been considered exclusively responsible for maintaining calcium homeostasis by regulating calcium, magnesium, and phosphate absorption to support bone health and growth. However, since vitamin D receptor (VDR) was discovered, more and more extra-skeletal effects of vitamin D have been identified. VDR has now been found present in almost all cells and organs in humans.
It has now been demonstrated that vitamin D plays important roles in cell proliferation and differentiation, regulates innate and adaptive immune responses, exerts anti-inflammatory activities, and has beneficial effects on neural development, lipid metabolism, and cardiovascular system, etc.
These diverse biological actions of vitamin D are regulated via ligand binding to VDR. Activated VDR complex can directly bind to specific DNA sequences called vitamin D response element (VDRE) that locates in the promoter region of vitamin D regulated genes and subsequently elicits downstream transcriptional regulation on those.
VDRE has been found in many genes, including vascular endothelial growth factor (VEGF) that regulates angiogenesis; proton-coupled folate transporter (PCFT) that regulates folate acid absorption and supports central nervous system development; forkhead box protein O1 (FOXO1) that regulates adipogenesis, gluconeogenesis, and glycogenolysis; and endothelial nitric oxide synthase (eNOS) that plays critical roles in protecting cardiovascular function by regulating vascular tone and exerts antithrombotic activity by inhibiting leukocyte adhesion and platelet aggregation. It is expected that more non-bone function of vitamin D will be discovered in the near future.
Beneficial effects of vitamin D in pregnancy
Although in 2010 the Food and Nutrition Board at the Institute of Medicine of the National Academies established that an adequate intake of vitamin D during pregnancy and lactation was 600 international units (IU) per day, higher vitamin D doses had been used in clinical trials to study the efficacy and safety in pregnant women. Reports from NICHD supported clinical trials conducted in South Carolina have shown that vitamin D supplementation of 4000 IU/day is safe and most effective in achieving sufficient 25(OD)D levels at 40-60 ng/ml (100-150 nmol) in pregnant women [8].
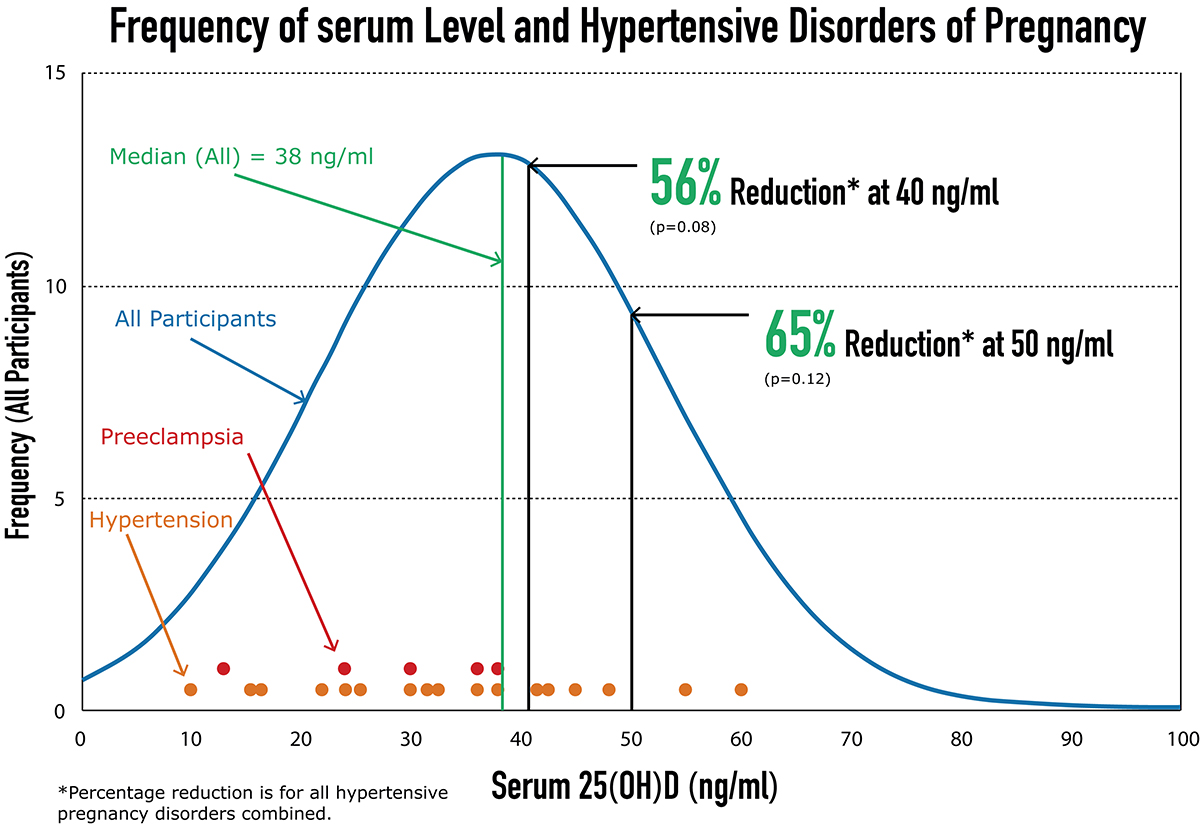
Most interestingly, their study also showed that women had 25(OH)D concentrations ≥40ng/ml had 56% lower risk of hypertensive disorders in pregnancy than those with <40ng/ml, and those who achieved 50ng/ml had 65% lower risk compared to those not (Figure 1). Furthermore, their study also demonstrated that maternal 25(OH)D concentrations ≥40 ng/ml were associated with substantial reduction of the risk of preterm birth [9]. Other studies also found vitamin D supplementation in pregnant women could reduce recurrent preeclampsia in those women who suffered from preeclampsia during their previous pregnancy [10].
Although inconsistent results were also reported from vitamin D supplementation trials in prevention of preeclampsia, the discrepancy could be due to the heterogeneric factors, including different baseline status of 25(OH)D, gestational age at clinical trial entry, different doses of vitamin D intake, and different metabolic responses to vitamin D in individuals during pregnancy. Since the cause(s) of hypertensive disorders/preeclampsia in pregnancy are heterogeneity in nature, future larger randomised control trials with vitamin D combined with low-dose aspirin and pravastatin are expected to improve the outcome of the preeclampsia preventive strategy in high risk population with vitamin D deficiency in pregnant women.
References
1. Hossein-nezhad A, Holick MF. Vitamin D for Health: A global perspective. Mayo Clin Proc 2013; 88: 720-755.
2. Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol 2009; 33: 130-137.
3. Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987-2004. Am J Hypertens 2008; 21: 521-526.
4. Fingar KR, Mabry-Hernandez I, Ngo-Metzger Q, et al. Delivery hospitalizations involving preeclampsia and eclampsia, 2005–2014. Statistical Brief #222. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs 2017.
5. Porreco RP, Barkey R. Peripartum intensive care. J Matern Fetal Neonatal Med 2010; 23: 1136-1138.
6. Khan KS, Wojdyla D, Say L, et al. WHO analysis of causes of maternal death: a systematic review. Lancet 2006; 367: 1066-1074.
7. Palmsten K, Buka SL, Michels KB. Maternal pregnancy-related hypertension and risk for hypertension in offspring later in life. Obstet Gynecol 2010; 116: 858-864.
8. Hollis BW, Johnson D, Hulsey TC, et al. Vitamin D supplementation during pregnancy: Double-blind, randomized clinical trial of safety and effectiveness. J Bone Miner Res 2011; 26: 2341-2357.
9. McDonnell SL, Baggerly KA, Baggerly CA, et al. Maternal 25(OH)D concentrations ≥40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center. PLoS One 2017; e0180483.
10. Behjat Sasan S, Zandvakili F, Soufizadeh N, Baybordi E. The effects of vitamin D supplement on prevention of recurrence of preeclampsia in pregnant women with a history of preeclampsia. Obstet Gynecol Int 2017; 8249264.
*Please note: This is a commercial profile











