A new study confirms that antimicrobial resistance increases as people travel internationally, with one scientist commenting that the world faces “a worrisome problem on the horizon”
Antimicrobial resistance is described by the World Health Organisation (WHO) as one of the top ten threats to humanity. Antimicrobial resistance (AMR) is when bacteria, viruses, fungi and parasites no longer respond to medicines – they evolve beyond what exists to stop them.
Diphtheria is one example, with over half of reported cases in 2018 happening in India. In a separate study, researchers found that the resistant genes in the disease were four-times higher in the 2010s than in the 1990s. The leap in resistance that happened over just 20 years is alarming in many ways – as the bacteria is also gaining clinical resistance to drugs not even used in diphtheria treatment.
The COVID pandemic has illustrated how crucial medicines are to the protection of human life, especially in countries which are yet to access the vaccine. This is one virus that has devastated the world. AMR involves the evolution of thousands of infectious diseases.
‘We’ve found numerous completely novel genes’, says first author
In this work, a team at the Washington University School of Medicine in St. Louis examined bacterial communities in the gut microbiomes of 190 Dutch adults before and after travel to one of four international regions – Southeastern Asia, South Asia, North Africa and Eastern Africa.
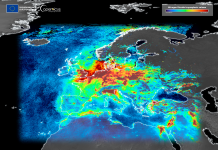
In these regions, the existence of antimicrobial resistance is high.
Alaric D’Souza, student at Washington University and a co-first author of the study, commented: “Even before the COVID-19 pandemic, we knew that international travel was contributing to the rapid global increase and spread of antimicrobial resistance. But what’s new here is that we’ve found numerous completely novel genes associated with antimicrobial resistance that suggest a worrisome problem on the horizon.”
The study was designed by co-senior authors John Penders, a medical microbiologist at Maastricht University, and Gautam Dantas, PhD, a professor of pathology & immunology at Washington University. Manish Boolchandani, PhD, a member of the Dantas Lab during the research and a 2020 graduate of the university’s doctoral program in Computational and Systems Biology, is also a first author on the paper.
56 unique antimicrobial resistance genes found
The team found 121 AMR genes across the gut microbiomes of 190 Dutch travellers. Interestingly, they had to use a highly sensitive technique to find all of them.
Over 40% of the genes they found were only noticeable via this sensitive examination, which presents a new problem – could other scientists who are not using these exact techniques be missing AMR genes? If so, what does that mean about accurate documentation of how fast such genes are spreading?
The scientists further found that 56 unique antimicrobial resistance genes actually became part of the travellers’ gut microbiomes while they were abroad. This includes several high-risk genes, like extended-spectrum β-lactamases (ESBL) and the plasmid-borne colistin resistance gene, mcr-1.
D’Souza further commented: “We found significant travel-related increases in the acquisition of resistance genes, abundance and diversity encoded by bacteria that are endemic to the region visited.
“These findings provide strong support for international travel as a vector for the global spread of clinically important antimicrobial resistance genes and highlight the need for broader surveillance of antimicrobial resistant bacteria in the gut microbiomes of returning travelers.”
But how is bacteria evolving this quickly?
According to their observations, the team noticed some behaviours between groups of organisms that allowed them to learn from one another – relatively quickly. Where there is a diverse bacterial community, AMR genes can be shared through something called ‘horizontal transfer’.
Horizontal transfer allows a snippet of DNA to jump from one to another, like a person changing trains.
Professor Gautam Dantas explained: “Since genes that code for resistance to different classes of antibiotics are often located on the same mobile elements, a single horizontal exchange has the potential to convert bacteria previously susceptible to antibiotics into a multi-drug resistant organism.
“Identifying new antimicrobial resistant bacteria and genes could play an important role in slowing the global spread of resistance and guide potential treatments for related diseases.”