John Greenwood PhD and Stephen E. Moss PhD explore the imminent potential of LRG1 as a microvascular dysfunction treatment
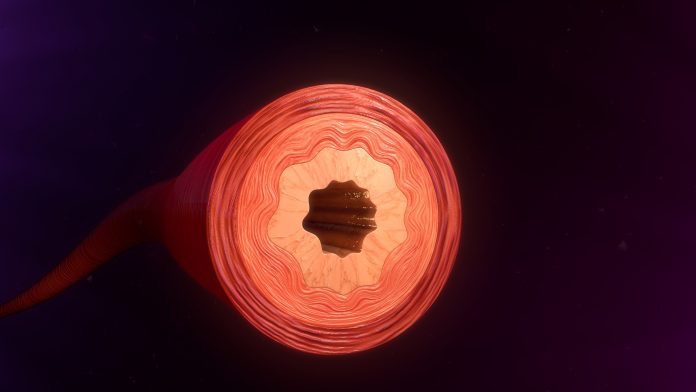
In many diseases the structure and function of blood vessels become compromised, resulting in a vasculature that either drives the pathology or contributes significantly to it.
Impaired vascular function
This may manifest either as dysfunction of existing vessels, where there is a loss of vascular stability, or in the formation of new vessels which fail to mature into a functional network, or both. Whatever the case, these diseased vessels are frequently leaky, haemorrhagic and often poorly perfused resulting in localised tissue damage, insufficient delivery of oxygen and poor access of therapeutic agents.
Therapeutic targeting of neovascularisation and vascular dysfunction
For many years there has been considerable focus on the vasculature of solid cancers, as the formation of new blood vessels (neovascularisation) is required for their growth and dissemination. Therapeutic targeting of the prototypic factor driving new blood vessel growth, namely vascular endothelial cell growth factor (VEGF), to restrict tumour vessel growth has delivered limited success. In eye disease, however, blocking the activity of VEGF has resulted in a step change in the treatment of wet (neovascular) age-related macular degeneration (AMD) and, increasingly, in vascular complications of diabetic retinopathy (DR). What has emerged from applications in the eye is that much of the clinical benefit derived from inhibiting VEGF is due to reversal of vascular dysfunction, or vessel normalisation, rather than restriction or ablation of new vessel growth.
This concept of normalising the vasculature in tumours, to improve vessel function, has gained considerable traction in recent years. This is based on the concept that abnormal vessels contribute to a pro-oncogenic tumour microenvironment, and their compromised function restricts delivery of therapeutics. As in the eye, where targeting VEGF improves vessel integrity, it has been proposed that in some cancers blocking VEGF activity may be used to normalise tumour vessels rather than inhibit their growth. This approach may have utility in other diseases, such as endometriosis, atherosclerosis, psoriasis and rheumatoid arthritis where new vessels are typically abnormal in structure and function leading to increased leakage, poor perfusion and haemorrhage – characteristics that underpin much of the pathology.
Whether one wants to prevent abnormal vessel growth, or return vessels to their normal state, therapeutic approaches to date have relied predominantly on targeting VEGF and its broader signalling network. What is clear, however, is that whilst the VEGF pathway is the major driver, many other factors are involved. This is best illustrated by the escape from VEGF dependency often exhibited by vessels in both cancer and ocular disease following inhibition of this pathway. Whilst this may be partly due to reliance on non-angiogenic processes, such as co-option of existing vessels, in many instances this resistance to anti-VEGF therapeutics is likely to be due to other factors playing a role in vascular growth and dysfunction. This is important, because the number of patients that are refractive to targeting the VEGF pathway is considerable and accordingly represents a major and seemingly increasing unmet clinical need.
In most diseases blood vessels lose normal function as part of the pathophysiological process but will often return to normal as tissues repair. This, however, doesn’t always occur and may leave vessels chronically dysfunctional. Moreover, and almost without exception, new vessel growth in diseased tissue occurs abnormally with persistent damaging vascular consequences. The mechanisms responsible for abnormal vessel growth are not entirely clear as many of the factors, such as VEGF, that drive neovascularisation are also involved in developmental/physiological angiogenesis. This suggests that in disease other pathogenic factors are generated that corrupt the normal angiogenic process, resulting in new vessels that fail to grow in a patterned manner, and fail to mature and stabilise as observed during developmental angiogenesis.
The secreted glycoprotein LRG1 disrupts blood vessels
New therapeutic targets are therefore urgently sought to meet the needs of the substantial population of patients that do not adequately respond to current vascular treatments. This imperative led our group to discover a new vascular destabilising factor that is overexpressed in diseased tissue1. This secreted glycoprotein, leucine-rich alpha-2-glycoprotein-1 (LRG1), interferes with the house-keeping activities of one of the most extensive biological pathways known, that of the transforming growth factor beta (TGFβ) family signalling network, resulting in failure of vascular stabilising mechanisms. Of clinical relevance, the TGFβ pathway is distinct from the VEGF signalling axis and therefore LRG1 represents a novel therapeutic target that may be responsible for driving VEGF-independent vascular dysfunction.
In health, LRG1 is expressed almost exclusively by the liver and neutrophils, but we and others have demonstrated that LRG1 is produced in abundance in many disease tissues, including those affecting the eye (wet AMD and DR), and in solid cancers. We have also shown that inhibition of LRG1 activity with blocking antibodies results in reduced neovascularisation, less vascular leakage and a more normalised vessel. In cancer models we have also demonstrated a vastly improved outcome when LRG1 blockade is combined with other therapeutics including cytotoxics or the emerging immunotherapies. The involvement of LRG1 in disease has also been corroborated in other experimental studies including, amongst others, diabetic kidney disease2 and pulmonary fibrosis3.
In support of these observations, there is now a considerable body of clinical evidence that LRG1 is associated with human disease, with publications rising exponentially. Again, this is especially true for cancers including, but not restricted to, colorectal, pancreatic, breast, ovarian, cervical, head and neck, lung and oesophageal, where circulating levels of LRG1 have been proposed as being both diagnostic and prognostic. Increased circulating levels of LRG1 are also associated with many other conditions such as diabetes, chronic kidney disease, ischaemia, lung disease, inflammation and infection, vasculitis, and psoriasis, supporting the idea that LRG1 may be a useful diagnostic biomarker.
In many studies, the increase in blood levels also correlated with disease severity and hence LRG1 is has been proposed as a potentially useful prognostic biomarker. Of particular interest, in the light of the current pandemic of COVID-19 caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is the increasing evidence that pulmonary microangiopathy, and more general microvascular dysfunction lie centre stage in the pathogenesis of the disease. Thus, the vascular pathology observed in the lung is also observed in other organs including the kidney, heart and brain. Intriguingly, a recent study has reported that in COVID-19 patients LRG1 is significantly upregulated, and along with other biomarkers can distinguish mild from severe cases4 prompting the authors to suggest that it may be prognostic and a viable therapeutic target.
LRG1 as a novel therapeutic target to improve vessel function
In all these conditions correlation does not infer cause, but the growing body of experimental evidence demonstrating that high levels of LRG1 causes vascular pathology, suggests that it may well be a significant pathogenic factor in these diseases and hence a potentially valuable therapeutic target. Accordingly, we have generated a humanised/deimmunised therapeutic antibody and Fab fragments for systemic and intraocular therapeutic delivery respectively with encouraging data on their safety and toxicology. In the coming few years we will be moving these into clinical trials in ocular disease and cancer and potentially into other indications. Time will tell whether therapeutic targeting of LRG1 will provide clinical benefit but the evidence that it will is growing year on year.
References
1 Wang X, Abraham S, McKenzie JAG, Jeffs N, Swire M, Tripathi VB, Luhmann UFO, Lange CAK, Zhai Z, Arthur HM, Bainbridge J, Moss SE, Greenwood J. LRG1 promotes angiogenesis by modulating endothelial TGF-β signalling. Nature. 2013 Jul 18;499(7458):306-11.
2 Hong Q, Zhang L, Fu J, Verghese DA, Chauhan K, Nadkarni GN, Li Z, Ju W, Kretzler M, Cai GY, Chen XM, D’Agati VD, Coca SG, Schlondorff D, He JC, Lee K. LRG1 promotes diabetic kidney disease progression by enhancing TGF-β-induced angiogenesis. J Am Soc Nephrol. 2019 Apr;30(4):546-562.
3 Honda H, Fujimoto M, Serada S, Urushima H, Mishima T, Lee H, Ohkawara T, Kohno N, Hattori N, Yokoyama A, Naka T. Leucine rich α2 glycoprotein promotes lung fibrosis by modulating TGF-β signaling in fibroblasts. Physiol Rep. 2017 Dec;5(24):e13556.
4 Messner CB, Demichev V, Wendisch D, Michalick L, White M, Freiwald A, Textoris-Taube K, Vernardis SI, Egger AS, Kreidl M, Ludwig D, Kilian C, Agostini F, Zelezniak A, Thibeault C, Pfeiffer M, Hippenstiel S, Hocke A, von Kalle C, Campbell A, Hayward C, Porteous DJ, Marioni RE, Langenberg C, Lilley KS, Kuebler WM, Mülleder M, Drosten C, Suttorp N, Witzenrath M, Kurth F, Sander LE, Ralser M. Ultra-high-throughput clinical proteomics reveals classifiers of COVID-19 infection. Cell Syst. 2020 Jul 22;11(1):11-24.e4. doi: 10.1016/j.cels.2020.05.012. [https://www.sciencedirect.com/science/article/pii/S2405471220301976]
*Please note: This is a commercial profile