Here, several academic experts explain what we need to know about removing the blindfold on antimicrobial resistance – by strengthening clinical microbiology laboratories in resource-limited settings
By any measure, antimicrobial resistance (AMR) is a global health emergency. Over 1.27 million deaths were attributable to AMR in 2019, a burden surpassing those of both HIV/AIDS and Malaria. By 2050, this toll is expected to increase to 10 million deaths per year and will dwarf the number of fatalities caused by malaria, tuberculosis, and HIV combined.
The existence of effective antimicrobials underlies the ability to perform complex medical procedures and care for people with cancer and critical illness. For each of these, infection is a major cause of death. Bluntly, virtually no aspect of modern medicine is possible without access to antimicrobials that work.
Currently, the highest rates of AMR are reported from low- and middle-income countries (LMICs). Of those, Sub-Saharan African countries are the least prepared to face the socio-economic costs of AMR. Several factors, including a focus on single-disease control programmes and health solutions sought via new technologies instead of human resources, have yielded neglect of overall health systems and many aspects of patient care.
The WHO’s Global Strategy for Containment of Antibiotic Resistance recognises that access to clinical bacteriology testing is a key bottleneck preventing individual patient management of treatable severe infections, detection of AMR, and implementation of effective antimicrobial stewardship (AMS) interventions. As a result, strengthening laboratory capacity became a focus of international efforts during the last decade. Unfortunately, progress has been slow.
As a complement to the article from Kozlakidis & Vandenberg, we describe our own experience implementing bacteriology laboratory capacity as the cornerstone of AMR containment activities in Ethiopia, and reflect on a need to fill the current vacuum between high-level recommendations and the reality of large parts of the LMIC healthcare landscape.
Antimicrobial use in LMIC
Even in urban referral centres, there is little access to bacteriology diagnostic testing in LMIC. The lack of diagnostic results means healthcare providers are working with a blindfold, unable to identify the specific infection a patient may be suffering from and unable to determine whether patients would benefit from antibiotics.
As a result, patients are often put on multiple, broad-spectrum antibiotics or prescribed antibiotics unnecessarily. This has led to significant overuse. For example, in Ethiopia, up to 85% of hospitalised patients are on antibiotics on any given day.
The importance of diagnostic testing
A study conducted with members of our group in North America quantified the loss of critical information when antibiotics were prescribed before microbiologic testing in patients with life-threatening infections. Among 325 patients with severe sepsis, approximately 50% of patients who had positive blood cultures before treatment had falsely negative cultures after administration of antibiotics. This signified that treatment could skew the detection of bacterial infection and underscored the importance of bacteriology testing before starting antibiotic treatment.
Prescribing antibiotics without a bacteriology diagnostic test massively reduces the sensitivity of blood cultures, which, in turn, reduces healthcare professionals’ ability to detect the specific source of bacterial infection.
To assess the clinical impact of such missed diagnoses, we performed blood-culture testing on 777 patients admitted to hospital in Ethiopia. Among these, the probability of having bacteria in the bloodstream was highest among patients who had received the most antimicrobials before testing – i.e. all patients for whom antimicrobials were prescribed as a “best guess”, instead of being informed by specific results.
Of greatest concern, around 80% of patients harboured bacteria resistant to the most prescribed drug, ceftriaxone. Having ceftriaxone-resistant bacteria in the blood was associated with a 15-fold increase in the odds of death. Earlier testing could have specified a more effective treatment by detecting these resistant bacteria.
Laboratory strengthening is feasible in low-resource settings with existing technologies
Despite international recognition of AMR and the value of diagnostic testing, solutions are not straightforward. High-level recommendations from WHO on AMR containment are frequently in direct conflict with local institutional priorities and the attitudes and experience of individual healthcare providers in LMICs. We worked with researchers from Addis Abba University to understand the factors needed to ensure sustainable change.
Through the Addis Ababa–McGill Partnership in Infectious Diseases, we conducted a project to strengthen the clinical bacteriology service at the Tikur Anbessa Specialised Hospital (TASH), the largest referral hospital in Ethiopia with approximately 20,000 admissions annually.
Using a relatively low-intensity 18-month intervention based on existing training tools and accreditation schemes, we demonstrate that the establishment of reasonable-quality clinical bacteriology is not only within reach, but also a critical step toward assessing the burden of AMR in settings like this one and implementing effective stewardship strategies. Taken together, all these measures resulted in a 50% reduction in antibiotic use in hospitalised patients.
Strikingly, the savings resulting from lower antimicrobial use were slightly greater than the annual cost of laboratory reagents, making the intervention financially feasible in addition to clinically beneficial.
Barriers to scaling-up bacteriology to remove the blindfold on AMR containment
The greatest barrier for containing the AMR global health emergency is adequate prioritisation at the policy level. This is true at all levels of governance. Gaining support from hospital leadership is required for changes in culture and sustainable practice. For example, demonstrating the clinical and financial impact of this work to policymakers yields the information they need to provide the appropriate budget and support to diagnostic bacteriology laboratories, so they can adopt routine quality-assured bacteriology testing as essential to AMR containment.
Beyond individual institutions, if clinical microbiology is recognised as a speciality in sub-Saharan Africa, expertise in this area can be fostered to produce a new generation of skilled microbiologists. Further, weak supply chains for bacteriology reagents, lack of comprehensive policies that address regulatory and fiscal obstacles for the diagnostic sector outside the laboratory, and a perennial lack of advancement opportunities for trained laboratory staff will require a strong collaborative effort and urgency from national- and hospital-level policymakers.
Acknowledgements
We are indebted to the numerous colleagues whose efforts have contributed to our evolving knowledge on optimal approaches to laboratory strengthening and implementation of antimicrobial stewardship in Ethiopia, including Gebremedhin Beedemariam, Temesgen Beyene, Michael Libman, Wondwossen Amogne, Solomie Deribessa, Daniel Seifu, Oystein Haarklau, the study and laboratory teams, and nursing and admin colleagues.
AMR: About our work
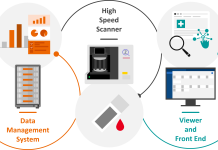
Our research programme aims to support global efforts towards better strategies for implementing bacteriology laboratories, to contain antimicrobial resistance (AMR) in low- and middle-income countries (LMIC). Our work evaluates specific laboratory tools or larger intervention bundles.
Examples include assessing rationalised “AMR toolkit” that can be scaled-up in LMIC, studying the diagnostic accuracy and clinical impact of new tools for AMR diagnostics as they become available or evaluating electronic decision support tools to help clinicians interpret key information at the point of antibiotic prescription.
We believe this work fills a current vacuum between high-level recommendations and the reality of large parts of the LMIC healthcare landscape.