People who survive COVID-19 pneumonia, take at least one year to heal their lungs, according to a study published in Radiology
While the vaccine gives the majority of people protection against hospitalisation and ICU, others exist outside of what vaccines alone can do. Some people are immunocompromised, have comorbidities or have less antibodies than other people – depending on when they received their last vaccination.
Now, some Governments expect their populations to incorporate COVID into their realities.
Long COVID continues to dominate the lives of some survivors. Individuals who leave ICU after the virus deal with a range of ongoing symptoms, which can impact various parts of the body. Among them, COVID-19 pneumonia is one of the most devastating.
“In the end, long-term follow-up, both clinical and radiological, is necessary to gather more information about the course and clinical role of persisting SARS-CoV-2 related chest CT abnormalities,” said study senior author Dr Gerlig Widmann, chief thoracic radiologist at Innsbruck Medical University.
Firstly, what is COVID-19 pneumonia?
According to Dr Rayman Lee, pulmonologist at Houston Methodist and not involved in this study: “Pneumonia occurs when a bacterial or viral infection causes significant damage and inflammation in the lungs. The resulting fluid and debris build-up makes it hard for a person to breathe — sometimes to such an extent that oxygen therapy or ventilator support is required.
“Regardless of the bacteria or virus causing it, pneumonia can become very serious, even life-threatening.”
COVID-19 pneumonia is different to ordinary pneumonia, where extensive damage to the lungs is caused by the coronavirus. The severity of COVID-19 pneumonia can mean the difference between life and death.
COVID-19 pneumonia harms lungs for one year after symptom onset
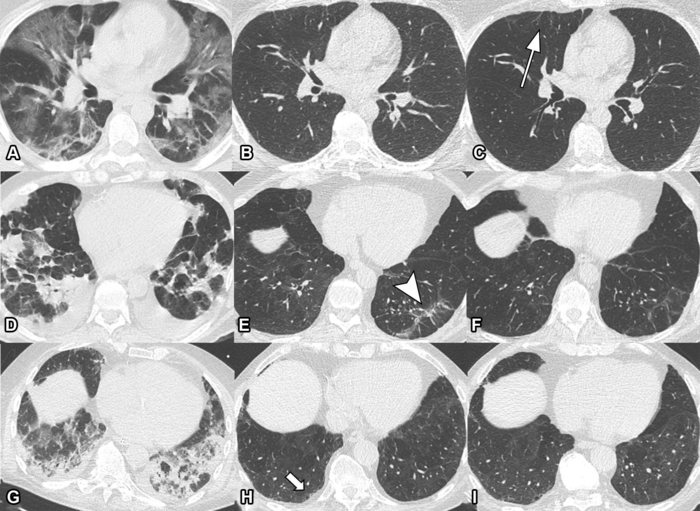
In this Austria-based observational study, researchers looked at the development of lung disease in patients with COVID. They looked at patterns and rates of improvement in chest abnormalities, especially in patients one year on from symptom onset.
CT scans, computed tomography, is a medical imaging technique used in radiology to obtain detailed internal images of the body for diagnostic purposes – completely noninvasively. When it comes to COVID survivors, CT scans are crucial to understanding how lungs are healing.
The scientists found that 63% of participants with abnormalities did not show further improvement after six months. Men, those aged over 60, and people with critical COVID-19 severity were most likely to still have lung abnormalities after one year.
“The observed chest CT abnormalities from our study are indicative of damaged lung tissue,” said study co-author Dr Anna Luger, from the Department of Radiology at Innsbruck Medical University in Innsbruck, Austria.
“However, it is currently unclear if they represent persistent scarring, and whether they regress over time or lead to pulmonary fibrosis.”











