Jitesh Patel, Project Director at Kajima Partnerships, discusses why the vaccine is not a silver bullet for longstanding pressures in elderly care and how the sector must adapt post-pandemic
The coronavirus pandemic has highlighted long-standing pressures on elderly living in the UK. Whilst the recent rollout of the Oxford/AstraZeneca vaccine is a promising step in relieving the impacts of COVID-19 on care homes, it is not a silver bullet. There remains a need to deliver specialist housing that utilises technology to strengthen a system of tiered care, relieving pressure on the NHS whilst supporting the wellbeing of residents now and beyond the pandemic.
Delivering new elderly care environments
COVID-19 has placed strain on elderly care services that were already operating under increasing pressure. The UK’s total population of over 65s is 12.4 million,(1) and the ageing population is set to exceed the growth in senior living housing stock, with one in four people expected to be over 65 by 2037.(2) Only 2.5% of the UK’s housing stock is defined as retirement housing, whilst the number of purpose-built homes offering care services comprises just 0.7% of the UK’s 29m homes. Evidently, new facilities are required to address a critical shortage of care residences.
The pandemic has also exposed the potential health risks of high-density environments. To address these changing priorities, appropriate solutions must be borne from innovative design. For example, clustered housing that offers ensuite accommodation alongside dining and living spaces shared between small groups will ensure that residents have private space but can also reap the social benefits of communal living. This model is particularly advantageous in an age of social distancing.
Tiered care
When building specialist elderly housing, it is essential to move beyond the one-level care home approach. Crucially, the spaces must offer a sense of community that has been found to be vital to wellbeing. More than 2.2 million people over 75 in the UK live alone, and Age UK states that there are now 1.4 chronically lonely people in England.(3) But this must also be matched by increased flexibility in care provision.
A tiered approach will allow residents to gradually upgrade their care as their needs increase, whilst the integration of community living facilities into residences will ensure that people remain actively involved with society. This combination will find the vital balance between privacy, dignity and community. Furthermore, investment in extra care independent living housing will offer many people moving into their senior years the option of accommodation that provides privacy and independence, whilst being close to care services, should they ever need them. This helps to alleviate anxiety and allows people to feel more safe and secure.
Service integration
In 2015, 20% of people reported feeling that they had not received the support they needed after discharge. More than ever, it is critical to ensure that people have access to step-down care. COVID-19 has amplified the pressures of bed-blocking that result from lack of integration between services during discharge. General and acute hospital bed numbers have declined by 34% since 1989, and healthcare services for the elderly continue to experience a spike in demand as a result of COVID-19 and routine winter pressures.
A report reviewing the government’s Care and Support Specialised Housing Fund recently recognised the significant benefits of developing specialist elderly housing, including alleviating pressure on the NHS.(4) A step-down approach that integrates out-patient services and community care providers will relieve healthcare services, whilst instituting appropriate and resilient spaces where people can continue their recoveries.
Leveraging technology
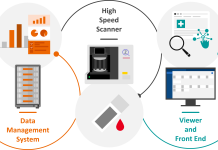
COVID-19 has also highlighted that many elderly living facilities sorely lack the digital capabilities to offer the most efficient care. We must utilise the opportunity provided by technology to reduce pressure on resources. Central databases of digitally held care notes can accurately track data and work alongside online consultations to provide optimum care. This digitisation will give vulnerable people access to virtual services from the safety of their own residences, thus navigating any potential issues if they are required to shield.
Importantly, technology can also improve standards of living for individuals. Wearable devices and motion activated facilities encourage a sense of autonomy whilst ensuring a safe living environment. Other technologies that enable contactless movement throughout residences – such as sensor-operated controls – will be impactful in minimising infection risk from surfaces in communal spaces.
An opportunity to deliver
COVID-19 has emphasised the need for innovation in approaches to long-term elderly care. News of vaccine rollouts are a welcome relief and should be celebrated – but this shouldn’t distract from the need to create accessible, technologically capable residences that integrate community services to encourage independence and wellbeing. By revolutionising the approach to elderly living environments, these residences will deliver support to both individuals and society long after COVID-19 has passed.
(3) https://www.ageuk.org.uk/our-impact/policy-research/loneliness-research-and-resources/#:~:text=There%20are%201.4m%20chronically,underpinned%20by%20evidence%20and%20data.