Peter Bretscher, Professor of Biochemistry, Microbiology & Immunology at the University of Saskatchewan, explores important immunological questions and how alternative frameworks can lead to effective progress in the field
Devising strategies of prevention and treatment of immune system-related diseases rests on two foundational, immunological questions. The frameworks used in attempts to address these questions over the last three decades are, I suggest, mistaken. Indeed, they result in classical observations being ignored to the detriment of progress. Here, I explain these assertions and indicate how alternative frameworks can lead to realistic interventions.
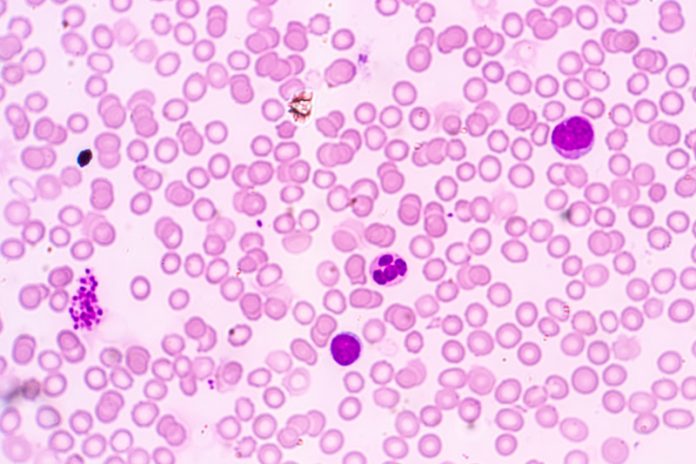
The immune system normally fights “foreign” invaders/antigens, but not parts of the body to which it belongs, the “self” antigens. Sometimes this attribute of “self-nonself discrimination” fails, resulting in “autoimmunity.” An example is autoimmune diabetes. The immune system also has two main means of attack, cell-mediated immunity (CMI) and antibodies. Moreover, it optimally generates these different classes of immunity under different circumstances. The two questions are:
- How do foreign and self-antigens interact differently with the immune system to respectively generate and ablate immune responses?
- What controls the class of immunity generated?
In other words, to be or not to be and, if to be, what to be?
These questions are pertinent to four areas of medicine:
- Autoimmunity.
- Infectious diseases.
- Cancer.
- Allergies.
I focus here on immunity to pathogens and cancers. Understanding immune class regulation is a prerequisite for developing strategies of prevention and treatment.
The dose of antigen and time after antigen impact were shown in the 1950s to affect the class of immunity generated. Low doses exclusively generate CMI. Medium doses generate CMI more rapidly, followed by antibody production and the down-regulation of CMI. High doses rapidly generate antibody responses; the cell-mediated phase may even be eclipsed. These observations hold generally. Early studies employed non-replicating, protein antigens. We demonstrated they also apply to immunity against live cancer cells and slowly growing intracellular bacteria and protozoa. Moreover, Parish showed in the late 1960s that the repetitive administration of low doses of a protein, that exclusively induces CMI, generates a “cell-mediated imprint.” Exposed animals, challenged with a high dose that induces antibody in unexposed animals, expressed stable CMI and produce little antibody. We demonstrated that cell-mediated imprints can be generated against live cancer cells and live bacteria and protozoa.
“The immune system normally fights ‘foreign’ invaders/antigens, but not parts of the body to which it belongs, the ‘self’ antigens.”
“Standard vaccination” ensures the vaccinated produce a more rapid, larger antibody response on infection. This is only effective against pathogens/invaders contained by antibody. Most cancers and some pathogens, such as those causing tuberculosis, AIDS, cutaneous and visceral leishmaniasis, are contained only by CMI. Disease is most often associated with predominant antibody responses. We made mice resistant to cancer and pathogens, uniquely susceptible to cell-mediated attack, by generating cell-mediated imprints. We call this the low-dose vaccination strategy.
My 1974 Theory of Immune Class Regulation explained how antigen interacts differently with cells of the immune system to generate CMI and antibodies. The theory accounts for the dependency of the cell-mediated/ antibody nature of the response on antigen dose and time after antigen impact. It also explained how cell-mediated imprints can occur. We have successfully tested predictions of this theory in diverse settings. Our studies on vaccination against cancer and pathogens uniquely susceptible to cell-mediated attack were based on the theory.
Janeway proposed in 1989 that a signal from innate defence is required to generate an immune response. Many later proposed such signals also determine the class of immunity generated. Such frameworks have been fleshed out by many cellular and molecular observations. These frameworks ignore and cannot explain many observations at “the level of the system”, such as the dependency of the cell-mediated/antibody nature of the response on antigen dose and time after antigen impact. The dominance of such questionable frameworks likely explains why reports showing the importance of antigen dose have received little attention. Jonas Salk, I and collaborators wrote a 1993 Science article on the low dose vaccination strategy against AIDS. I now illustrate the potential of our framework for treatment by describing a proposed personalised therapy of HIV-1 infection.
Immune responses naturally evolve from a cell-mediated to an antibody mode. Treating a patient, ill through infection by a pathogen uniquely susceptible to CMI, requires the response to be modulated in the reverse direction. Visceral leishmaniasis is caused by such a pathogen. Treatment of this otherwise lethal disease is via a short course of anti-parasite drugs. This treatment modulates the response from predominant antibody production to predominant CMI. The drugs kill the parasite and thus reduce the antigen load. Treated individuals are resistant to reinfection! These, and other findings, led us to propose that the level of antigen not only affects the cell-mediated/antibody nature of primary but also ongoing responses.
“Immune responses naturally evolve from a cell-mediated to an antibody mode.”
About 1% of HIV-1 infected individuals generate stable CMI, “the elite controllers.” These individuals produce either no IgG antibodies or predominantly IgG2 antibodies indicative of a predominant cell-mediated response. Most other infected individuals are given anti-retroviral therapy (ART). Cessation of therapy usually results in rapid viral rebound. Long-term ART, by dramatically reducing viral and so antigen load, undermines all immunity in most individuals. About 15% of individuals, on ART for three years, do not suffer viral rebound on cessation of therapy, the “post-treatment controllers.” We and others suggest that the virus is kept at very low levels due to protective immunity. The instigation of ART reduces viral levels and the antigen load. We argue that the anti-HIV-1 immunity of all individuals put onto ART will evolve with time from a mixed cell-mediated/antibody to a predominant cell-mediated mode, as occurs in the treatment of visceral leishmaniasis. Treated visceral leishmaniasis patients predominantly produce IgG2 antibody, indicating predominant CMI. Cessation of ART when anti-HIV-1 IgG2 antibodies are predominant is expected to result in viral containment. Further ART at this time would further lower the level of the virus and so undermine the generation of all immunity. We, therefore, propose that cessation of ART will only result in viral containment around the time when the anti-HIV-1 IgG2 antibodies are predominant. Such individuals will not only be cured but will be minimally infectious. This strategy provides hope, if implemented, in containing and resolving the AIDS pandemic. Similar strategies may allow the optimal harnessing of patients’ protective immunity against some cancers, as most treatments reduce the antigen load.