A group of experts from ISBER shed light on the science of biobanking and its role in delivering modern and precision medicine
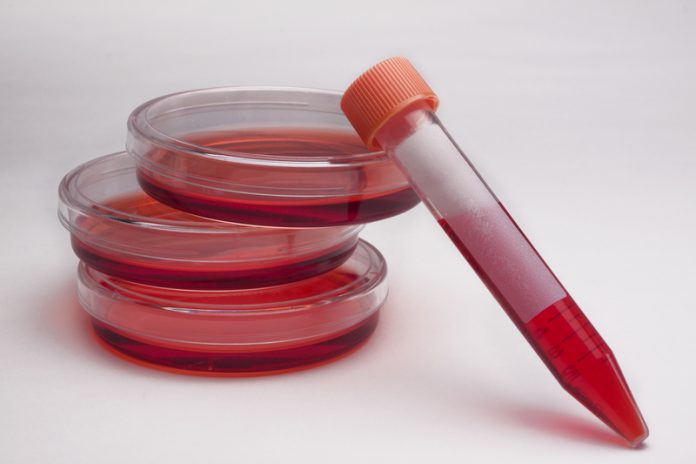
Twenty years ago, an internet search for the word “biobank” would have returned almost nothing; today, there are millions of results. The term biobank commonly refers to a large collection of tissue samples (with associated biological and medical data), such as surgical biopsies (fresh frozen or in paraffin sections), blood and serum samples, different cell types, DNA, RNA; all carefully collected for research purposes. (1) The science of biobanking is very broad and covers collections of plant, animal, or human specimens. For the purposes of this discussion, we will focus on human biobanks.
Two decades is a very short period of time, for a concept that has become vital to delivering modern, precision medicine – both in terms of research and the clinic itself. One of the first biobanking initiatives came from the Organization for Economic Cooperation and Development (OECD), which advocated the importance of biobanks, but also insisted on the need to have an accreditation system. (2)
In the years following this OECD proposal, various countries began establishing biobanks as research infrastructure. Thus, many national biobanks and biobank networks were created in Canada, the UK, USA, China, Estonia, South Korea, Finland, Denmark, Sweden, France and many other countries. In our opinion, biobanks crucially underpin and facilitate the national and international medical research efforts, by providing high-quality, research-ready samples. In addition, biobanks are linked to clinical data for investigators, according to a set of best practices and standards.
In 1999, the International Society of Biological and Environmental Repositories (ISBER) was formed(www.isber.org). Since then, academics, biobankers, NIH Institute representatives, patient advocates, industry representatives, lawyers and others with an interest in biobanking meet annually at the ISBER Annual General Meeting, to share their expert knowledge in the field.
In 2005, ISBER developed and published the Best Practices for Repositories, which was revised at regular intervals and translated into many languages. We are currently anticipating the fourth edition should be published late in 2017. (3)
This is the premier ‘handbook’ for biobanks to achieve quality products in their laboratories. Topics such as cost recovery, facilities, equipment, safety, quality assurance and quality control, ethical issues, specimen collection, processing, and retrieval, training, specimen culling, and much more are discussed. ISBER’s journal, Biopreservation and Biobanking, is a well-established, international peer-reviewed journal, that highlights vital research in the field. (4)
The road to precision medicine
Medical research in the era of precision medicine is based on the analysis of samples with clinical data – and, because the associations are often weak, we need these samples in large quantities. The implication is clear: if more, well-characterised, high-quality samples are available through biobanks, the faster research will advance and impact upon the faster delivery of healthcare today. However, to fulfil the aim of precision medicine, challenges remain on the road ahead.
Standards and harmonisation
The most important aspects of a biobank are consistency and quality. The validity of the data generated by biobanked samples depends on their quality, which is in turn dependent on the use of stringent standards in collecting the biospecimens and delineating patient characteristics. Variations associated with collecting, processing and storing different samples and the accompanying clinical data, make it extremely difficult to extrapolate or to merge data from different studies. Without that information, it’s easy to introduce invisible bias into the work, leading to irreproducible work! Therefore, the standardisation and harmonisation of biobanking practices are of paramount importance.
Data and ethics
As medical researchers “think bigger” than ever before, their need for data grows ever stronger. It demands the gathering and administration of large collections of samples and related data, often from multiple sources. This is not an endeavour for individuals, single projects, or small research groups, because of the high costs in time, sample access, technological resources and the funding involved. Hence, ‘virtual biobanks’ started forming with institutional collaboration and geographically distributed forms of endeavour. One such major collaborative effort is the Biobanking and Biomolecular Resources Research Infrastructure (BBMRI-ERIC). (5) The pan-European BBMRI vision emerged from the recognition that keeping up with policies and developments elsewhere, most notably in the USA, necessitates integrated European research.
These “big data” approaches in precision medicine require access to personal and often identifiable information and are coupled with ethical challenges. For example, the ‘big data’ complexity may impact informed consent; or the need/ability to return the outcomes of test to the patients who originally donated their samples. Considered together, a constructive and transparent inclusion of ethical questioning in this rapidly evolving field is necessary to support the societal acceptance and responsible development of the technological advancement.
Costs and sustainability
The aspect of biobank sustainability is critical for precision medicine research. Recent advances in health research (including social and public health research, and advances in technology) have increased demands on the types of samples and processing provided by biobanks.
Specifically, researchers require increasing sample numbers and associated clinical data, biobanks increasingly implement standardised processes to attain higher quality standards, while funders seek performance metrics and assurances for their investments. Research funding agencies, institutions and philanthropic organisations, often assume that beyond the initial start-up operational and infrastructure costs that biobanks at some point should be become “self-sustaining.”
This is rarely achievable in the context of planning a large national infrastructure with a 15- to 20-year life cycle even with governmental or institutional funding, and it does not represent most biobanks attached to integrated academic/health institutions or disease-focused biobanks, such as those assisting with rare genetic conditions research. (6) Thus, new or more flexible operating and funding models are needed to support the growth of biobanking in the medium and long-term.
References
(1) Parodi B. (2015) Biobanks: A definition. In Ethics, Law and Governance
of Biobanking, Mascalzoni D. (ed.), The International Library of Ethics,
Law and Technology 14, Springer Science and Business Media
Dordrecht 2015. DOI 10.1007/978-94-017-9573-9.
(2) Organization for Economic Co-operation and Development (OECD).
(2006) Creation and Governance of Human Genetic Research
Databases. OECD Publishing: Paris.
(3) ISBER Best practices for repositories: Collection, storage, retrieval, and
distribution of biological materials for research. (2012) Biopreserv
Biobank; 10:79-161.
(4) www.liebertpub.com/overview/biopreservation-and-biobanking/110/
(6) Watson PH, Nussbeck SY, Carter C, et al. (2014) A framework for
biobank sustainability. Biopreserv Biobank; 12:60–68.
Zisis Kozlakidisa
Division of Infection and Immunity, University College London, United Kingdom
David Lewandowskib
Brooks Life Science Systems. Chelmsford, United States
Brent Schacterc
CancerCare Manitoba/University of Manitoba, Winnipeg, Canada
International Society for Biological and Environmental Repositories (ISBER)
Tel: +1 604 484 5693