Matt Elcock, Founder/Managing Director of Push Doctor, charts the road ahead when it comes to how digital solutions will support the NHS’s recovery
After the ordeal of COVID-19, clinicians and patients can be forgiven for believing the NHS’s road to recovery will be a long and complex one. They are right. The pandemic has tested all parts of the health service to its limits and beyond, from hospital staff fighting the virus through to GPs supporting patients whose lives have been put on hold by delays to care elsewhere in the NHS. There is no quick fix to the pre-existing and longer-term demographic, funding and structural pressures that have been exacerbated by COVID-19. But as we move beyond the pandemic and begin to live alongside the virus, it is time to consider how digital can support the NHS on its path forward.
The pandemic has accelerated changes to how we use technology, with healthcare being no exception. One of the ways this has played out is via the steep growth of virtual healthcare. As people were encouraged to stay home to reduce the spread of COVID-19, clinicians quickly pivoted to carry out more of their patient interactions via video. At the height of the pandemic, NHS Digital estimated that around half of the 102 million GP appointments took place over the phone or via video call. Fast forward to today and clinicians are reporting increased patient demand for remote services and greater momentum behind digital transformation projects.
The NHS workforce
In primary care, the cornerstone of our health system, staff are experiencing high levels of burnout, with as many as 36% of GPs considering early retirement. Demand for appointments has also skyrocketed, leading to increased pressures and an unmanageable workload. The capacity crisis needs to be addressed urgently, which is where I see the power of digital coming into its own. Digital solutions can help clinicians better manage demands on their time by providing thousands of additional video appointments. This allows GPs to focus on delivering face-to-face care to patients that really need it, while pressing ahead with the vaccination programme. Crucially, the cost of these digital appointments is significantly lower for the NHS, with savings of as much as 33% on the cost of a face-to-face appointment.
With an already overstretched primary care workforce, ensuring that patients are immediately directed to the right clinician to help them recover has never been more important. It is estimated that one-third of GP appointments could be completed by pharmacists who are trained to treat minor ailments such as coughs, colds, aches and pains. Digital solutions can help triage patients more effectively based on their medical records and symptoms so they are put in front of the right clinician at the right time, be that a doctor, physiotherapist, pharmacist, or another clinician type. This, in turn, reduces demand on GP surgeries and enables general practitioners to deal with more complex cases face-to-face.
The recruitment and retention of primary care staff across the board pose an ongoing challenge for the NHS. A digital medical workforce can help solve this problem by enabling clinicians from across the country to consult remotely with patients via video call, significantly increasing the pool of medical professionals available to a local surgery. Digital providers can support clinicians, practice staff and patients by providing these triage tools and bolstering the primary clinician team with a digital workforce.
Accessing technology for healthcare
Despite the acceleration of digital services due to COVID-19, there are still many patients who struggle to access the internet and smartphones – and patients facing these barriers must not be left behind. Widening and equalising access to healthcare through digital goes hand in hand with reducing pressure in certain pockets of the NHS, such as primary care. That’s why as an industry, we must work together to prevent people from experiencing differences in healthcare based on factors often outside their control and enable everyone to share in the benefits of digital. Alongside this, it is often the case that deprived and/or rural areas have fewer GPs per head than their more affluent counterparts, known as ‘underdoctored’ areas, meaning it is harder for patients to see a clinician when they need to. Digital healthcare solutions have the opportunity to play an important role in addressing this challenge by creating a location-agnostic workforce.
Embedding greater interoperability within the NHS is another area that will be crucial in its post-pandemic recovery. Despite some progress, digital bureaucracy still exists across the service. In some cases, hundreds of different systems operate in a single organisation or NHS Trust, and they often struggle to work in harmony. Poor interoperability prevents clinicians from accessing a patient’s information at the point of need, for example, a GP may want to prescribe medication for back pain but cannot see which painkillers that patient was given at a recent hospital visit. While it may not always be front of mind for patients, better interoperability translates to better health outcomes across the board, making consultations safer, more effective and efficient.
Closing remarks
With the pressures of increased demand, delivering the vaccination programme and supporting the backlog of patients on waiting lists for services elsewhere in the NHS, primary care is at a critical juncture. The pandemic has shown us how digital technology can help, working alongside face-to-face care to make systems more sustainable, efficient and joined-up, with clear benefits for clinicians and patients alike.
Data in healthcare for patients & staff
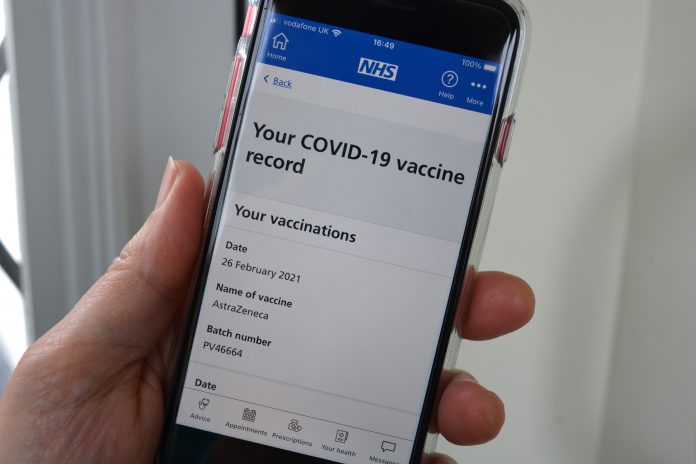
‘Data Saves Lives: Reshaping health and social care with data’, a draft strategy published by NHSX on 22nd June 2021 takes the remarkable use of data during the COVID-19 pandemic a step further with the security and privacy of data at the core. Included in the proposals, patients can access their test results with ease and care plans from all parts of the health system using patient apps, like the NHS App. Ensuring data is shared more effectively and safely across the system is important here. Improving access to data enables one to refill medications and speak with health and care staff, for instance.
Matthew Gould, NHSX Chief Executive, provides further insight concerning how data saves lives. “Throughout the pandemic we saw examples of data improving care and saving lives – from the speed of vaccine development to the discovery of treatments for COVID-19. If we want to continue improving care, we need to transform how we use data.
“Patients need to own their data, have access to their data, and have confidence on how the NHS is handling it on their behalf. This strategy takes this agenda firmly forward, and is good news for patients, staff, citizens and anyone who cares about the future of the NHS.” (1)
England’s Chief Nurse announced on 17th June that every mum can access their maternity records on smartphones. Dr Simon Eccles, Chief Clinical Information Officer and Deputy Chief Executive of NHSX, explains what this means for pregnant women and those who care for them: “Ensuring that every pregnant woman and all the clinicians caring for her can see the same crucial health information about their own care and unborn child is essential. That is why we are prioritising this work to put shared maternity records in all parts of the country as quickly as possible.” (2)
References